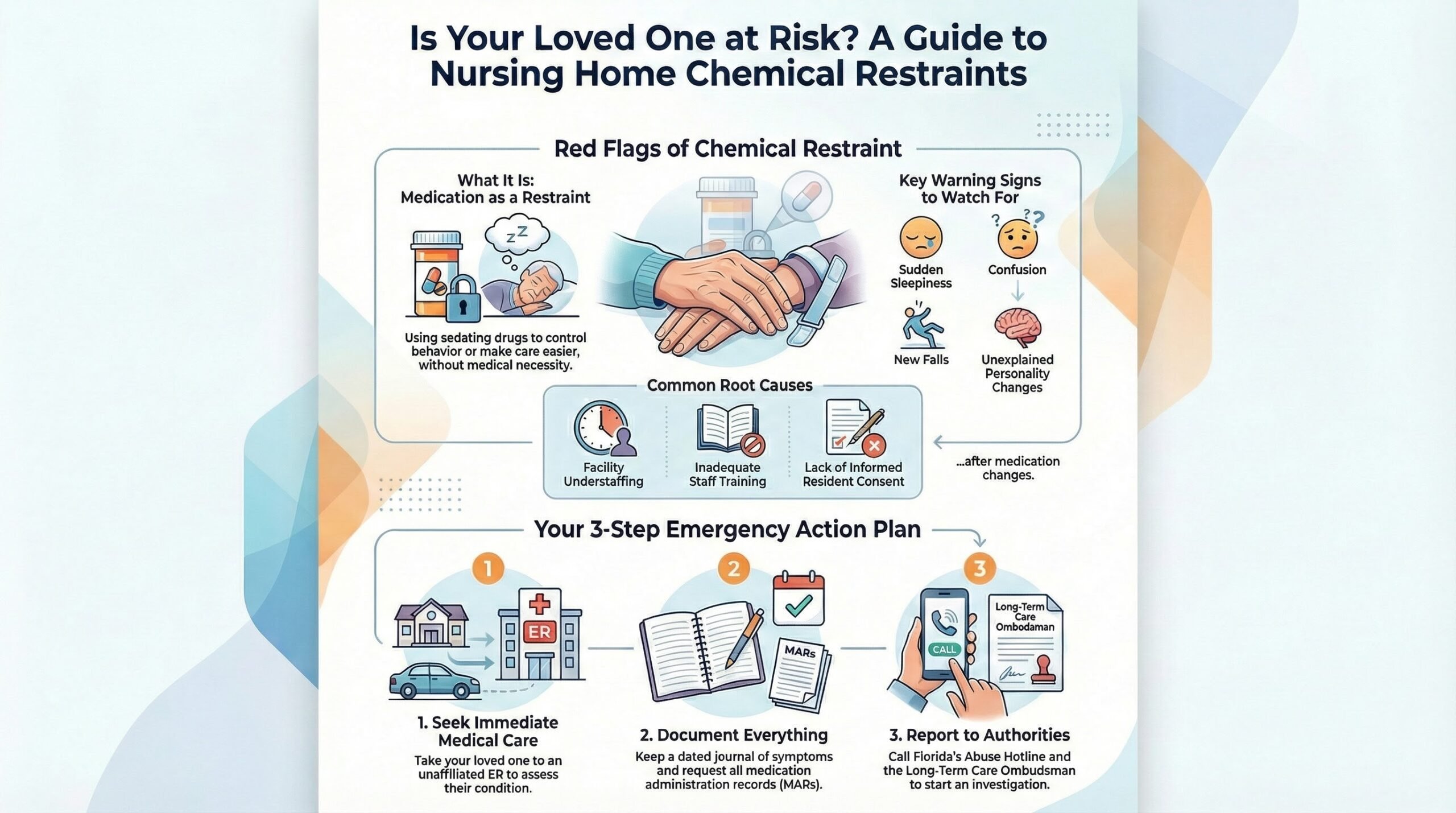
If you suspect a Fort Lauderdale nursing home is using sedating drugs as chemical restraints for staff convenience, you can act quickly to protect your loved one and any potential legal claim.
Request an immediate review of all medications, changes to the care plan, and copies of medication administration records (MARs), physician orders, and any consent forms.
Carefully document any sudden sleepiness, confusion, unexplained falls, or personality changes, and seek emergency medical care if symptoms appear dangerous.
You should also report your concerns to the appropriate Florida authorities.
To understand your legal options and how the Law Offices of Anidjar and Levine can assist, speak with a Fort Lauderdale Nursing Home Abuse and Neglect Lawyer.
Key Takeaways
- Chemical restraint abuse involves sedatives used for staff convenience, without documented medical need or informed consent, causing harmful overmedication.
- Seek immediate medical evaluation for severe sedation, confusion, breathing issues, or falls, preferably at an unaffiliated ER or urgent care.
- Preserve evidence by requesting medication lists, MARs, orders, PRN logs, consent forms, and keeping a dated symptom journal with photos.
- Report suspected abuse to Florida’s Abuse Hotline, the Long-Term Care Ombudsman, and AHCA to trigger oversight and preserve facility records.
- A Fort Lauderdale chemical restraints abuse lawyer can secure records, identify authorization failures, interview witnesses, and pursue claims for injury and rights violations.
How We Can Help With Your Fort Lauderdale Nursing Home Chemical Restraints Abuse Claim
When you reach out, we’ll step in quickly to protect your loved one and start building a strong Fort Lauderdale chemical restraints abuse claim.
You’ll get clear guidance on immediate safety steps, including requesting care plan changes and documenting medication effects.
We’ll help you gather records, preserve evidence, and identify who authorized the drugs and why.
You’ll never feel left in the dark. We’ll use practical communication strategies so you can speak with administrators, nurses, and physicians with purpose and calm authority.
We’ll coordinate family support by aligning relatives around a single plan, delegating tasks, and keeping everyone updated. You’ll also receive help organizing timelines, witness statements, and photos, so your story stays consistent.
If the facility pushes back, you’ll have someone who can challenge excuses, demand answers, and pursue accountability. You focus on your loved one’s dignity; we’ll handle the legal pressure and next steps.
Understanding Fort Lauderdale Nursing Home Chemical Restraint Abuse Cases
Although some facilities describe sedating medications as “for agitation” or “to keep residents safe,” chemical restraints abuse happens when drugs are used to control behavior or make care easier instead of treating a documented medical need. You can best serve your loved one by recognizing what this looks like in real life: a sudden change in alertness, mobility, speech, or personality after new or increased psychotropic medications.
| What you notice | Why it matters |
|---|---|
| Unusual sleepiness or “zoned out” behavior | May signal overmedication, not care |
| New falls or trouble walking | Sedation can raise injury risk |
| Less conversation or interest | Can undermine resident autonomy |
You help protect dignity by asking for the care plan, medication list, and the clinical reason for each drug. In Fort Lauderdale, strong cases often focus on documentation gaps, informed consent issues, and whether staff adhered to medication ethics and resident-centered goals.
Common Causes of Fort Lauderdale Nursing Home Chemical Restraint Abuse
You’ll often see chemical restraints misused when a Fort Lauderdale facility is understaffed, and staff choose convenience over proper care.
Abuse can also stem from improper medication management and giving drugs without your loved one’s informed consent.
When staff training falls short, they’re more likely to rely on sedating medications instead of safer, individualized interventions.
Understaffing And Convenience
Understaffing often drives chemical restraint abuse because overworked nursing home staff may rely on sedating medications to control residents faster than they can provide hands-on care.
When Staffing Ratios fall short, you may see residents labeled “difficult” instead of supported with patience, redirection, and dignity. That shortcut can quietly replace meaningful engagement, mobility assistance, and timely toileting—needs that require time and teamwork.
Convenience also shows up when a facility prioritizes routines over residents’ individual rhythms. You might notice fewer activities, rushed meals, and delayed call-light responses, all signs that Care Quality is slipping.
If you serve residents or advocate for families, push for staffing accountability, person-centered schedules, and non-drug calming approaches that honor each person’s rights and safety every day.
Improper Medication Management
When a facility leans on convenience and rushed routines, medication practices often slip, and that’s where chemical restraint abuse can take hold. You can see it when staff skip careful monitoring, don’t adjust dosages, or treat agitation with sedating drugs instead of addressing pain, infection, or anxiety.
If the team fails at medication reconciliation, they may miss duplicative prescriptions, dangerous interactions, or discontinued orders that linger on charts. Pharmacy errors can include the wrong medication, wrong strength, or unclear directions, and busy staff may administer it anyway. You help protect residents when you insist on accurate records, timely physician review, and documented, symptom-based alternatives.
When management ignores red flags, repeated overmedication can become routine, turning a clinical tool into a shortcut that harms the people you serve.
Lack Of Resident Consent
Skipping resident consent turns a medication order into a chemical restraint. When you give sedating drugs without a clear, voluntary “yes,” you override patient autonomy and risk silencing the person you’re meant to protect.
Consent isn’t a signature shoved across a table; it’s a real conversation about purpose, benefits, side effects, alternatives, and the right to pause or decline. I
f a resident can’t communicate, you still must seek input from a lawful surrogate and document why the medication’s necessary now.
Watch for red flags: meds started after complaints, doses increased to “keep them calm,” or refusals ignored.
Respecting informed refusal honors dignity and builds trust, even when care feels urgent. It also supports safer, more ethical outcomes for everyone.
Inadequate Staff Training
Consent failures often trace back to a deeper problem: staff who haven’t been trained to recognize chemical restraints or handle challenging behaviors without reaching for sedating meds. When you’re short on practical instruction, you may mistake dementia-related agitation for “noncompliance” and accept PRN orders as routine. You can prevent harm by insisting on competency assessments, coaching, and clear escalation steps that protect dignity.
| Training gap | Safer response |
|---|---|
| Mislabeling agitation | Use de-escalation scripts |
| Weak med knowledge | Flag restraint-like side effects |
| No scenario practice | Build simulation training drills |
| Poor documentation | Record triggers, alternatives, and outcomes |
When you commit to skill-based learning, you support residents’ freedom, reduce falls, and honor families’ trust—without relying on chemical control.
Legal Rights of Fort Lauderdale Nursing Home Chemical Restraints Abuse Victims
Although a nursing home might claim it used medication to “keep your loved one calm,” Florida law gives you clear rights if staff relied on chemical restraints for convenience instead of a legitimate medical need.
You can demand dignity, informed consent, and care plans that prioritize safety, not sedation, under Resident Rights standards.
You also have power through Family Advocacy: you can ask questions, insist on transparency, and push the facility to honor physician oversight and the least-restrictive alternatives.
Picture what those rights protect:
- A bedside chart that clearly explains every dose, purpose, and duration.
- A care conference where you’re heard and your loved one’s wishes guide decisions.
- A medication review that flags overuse, interactions, and sudden behavior changes.
- A calm room where comfort measures replace “quieting” drugs.
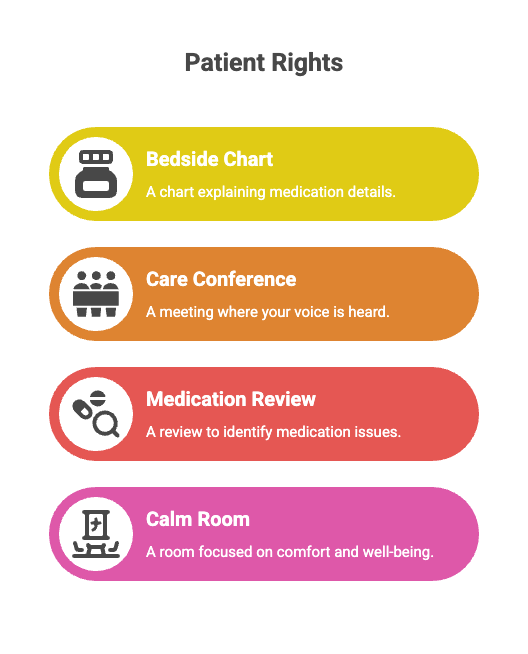
If the home violated these protections, you can pursue accountability, damages, and corrective action to safeguard others as well.
Steps to Take After a Fort Lauderdale Nursing Home Chemical Restraints Abuse
If you suspect chemical restraints abuse in a Fort Lauderdale nursing home, get your loved one immediate medical care to address dangerous side effects and stabilize their condition.
Document the medications given, dosage changes, and any symptoms you observe, and keep copies of records and photos if you can.
Then report the abuse to the appropriate authorities right away so an investigation can start quickly.
Seek Immediate Medical Care
When you suspect a nursing home used chemical restraints, get your loved one medical care right away to protect their health and create a clear record of what happened. Call 911 if they’re hard to wake, struggling to breathe, or suddenly confused.
Ask for an emergency evaluation to check essential signs, oxygen levels, and medication effects, and to rule out stroke, infection, or overdose.
If you can, have them taken to an ER or urgent care not affiliated with the facility. Tell clinicians about recent medication changes, missed doses, or unusually strong sedation.
Request immediate stabilization if they’re dehydrated, hypotensive, or at risk of falls. Stay with them, advocate calmly, and ensure they’re treated with dignity and compassion throughout their care.
Document Abuse And Symptoms
After you’ve gotten your loved one checked and stabilized, start documenting everything you’re seeing and hearing, because details can fade fast and the facility’s story may change.
Keep a dated journal of symptoms like sudden sleepiness, confusion, falls, slurred speech, tremors, or personality shifts.
Do focused behavioral observation: note triggers, staff interactions, and how long sedation lasts after visits or meals.
Ask for medication lists, MAR entries, dosage changes, PRN orders, and consent forms, and start medication monitoring by logging times given versus effects you notice.
Photograph bruises, skin breakdown, and unsafe conditions, and preserve clothing or pill packaging if you receive it.
Save voicemails, emails, and visit notes, and write down the names and roles of everyone you speak with.
Report To Authorities Promptly
Once your loved one’s immediate medical needs get addressed, report suspected chemical restraint abuse right away so the facility can’t quietly rewrite the narrative or “correct” records.
Make immediate reporting part of your care plan: call Florida’s abuse hotline, notify the Long-Term Care Ombudsman, and request a police welfare check if you fear imminent harm. Ask for a report number and the investigator’s name.
You can also contact the Agency for Health Care Administration to trigger an inspection and preserve medication administration records, orders, and staffing logs.
If a staff member confides in you, encourage them to speak up; remind them that Florida recognizes whistleblower protections and retaliation is unlawful.
Stay calm, stick to facts, and follow up in writing so your advocacy helps your loved one and protects other residents, too.
How a Fort Lauderdale Nursing Home Chemical Restraints Abuse Lawyer Can Help You
Although nursing homes may claim sedatives or antipsychotics “keep residents calm,” chemical restraints often signal neglect or outright abuse, and you don’t have to accept their explanation.
A Fort Lauderdale nursing home chemical restraints abuse attorney helps you act with purpose, protect your loved one, and honor Medication ethics through clear, lawful steps.
You’ll get guidance that strengthens Family advocacy while keeping the focus on compassionate care.
- Review the chart like a lantern—your lawyer requests records, orders, and consent forms to spot missing approvals.
- Interview witnesses like a steady compass—staff, residents, and visitors can confirm patterns of overmedication.
- Bring in experts like a clean window—pharmacology and nursing consultants explain proper dosing and alternatives.
- Pursue accountability like a firm handrail—your lawyer demands policy changes, negotiates compensation, and, if needed, files suit to stop the practice.
Long Term Effects of Fort Lauderdale Nursing Home Chemical Restraint Abuse Injuries
When a Fort Lauderdale nursing home relies on chemical restraints, you can face lasting harm that doesn’t fade when the medication stops.
You may see cognitive decline that speeds up dementia, along with sedation that raises your risk of falls and fractures.
You can also experience emotional and behavioral deterioration that leaves you withdrawn, agitated, or harder to care for.
Cognitive Decline And Dementia
Even if staff claims a sedative “keeps your loved one calm,” chemical restraints can speed up cognitive decline and worsen dementia symptoms over time.
You may notice increased confusion, dulled attention, and reduced ability to communicate needs, which can erode dignity and connection. These drugs can also mask pain, dehydration, or infection, delaying proper treatment and letting decline deepen unnoticed.
When you serve your loved one, you advocate for care that supports alertness, routine, and purpose. Request regular cognitive assessments, document changes you observe, and ask whether the facility has a memory care plan tailored to triggers, sleep, and meaningful engagement.
If staff rely on sedation instead of supervision and therapeutic approaches, you can challenge that choice and seek accountability for harm.
Increased Fall And Fracture Risk
As sedatives dull balance and slow reaction time, they raise your loved one’s risk of dangerous falls that can lead to lasting injuries. When staff rely on chemical restraints, you may see unsteady walking, dizziness, low blood pressure, and delayed reflexes—common Medication side effects that turn routine transfers into emergencies.
A single fall can cause hip fractures, head trauma, bleeding, or complications that steal mobility and independence.
You can serve your loved one best by asking for documented Balance assessments, fall-risk scoring, and a clear plan to reduce sedating drugs. Insist on safer supports, such as assisted ambulation, bed and chair alarms, proper footwear, and frequent rounding.
If the facility ignores preventable risks, you can hold it accountable and protect others from the same harm.
Emotional And Behavioral Deterioration
Although the drug may quiet a resident in the moment, chemical restraints often trigger emotional and behavioral deterioration that lasts long after the dose wears off. You may notice a once-engaged elder becoming distant, fearful, or irritable, with mood swings that caregivers mislabel as “progression.” When sedation blunts awareness, your loved one can lose confidence, stop initiating conversation, and slip into social withdrawal that deepens depression. You can serve them best by tracking changes, asking for medication rationale, and requesting non-drug supports.
| What you observe | What it may signal | How can you respond |
|---|---|---|
| Flat affect, silence | Over-sedation | Request dose review |
| Agitation, tears | Anxiety from restraint | Ask for calming routines |
| Isolation, refusal | Loss of autonomy | Advocate for engagement |
Proving Liability in Fort Lauderdale Nursing Home Chemical Restraints Abuse Cases
When you suspect a Fort Lauderdale nursing home used chemical restraints to control a resident, proving liability starts with showing the drugs weren’t medically necessary, and the facility chose convenience over care.
You’ll focus on whether staff medicated to manage behavior, reduce staffing demands, or silence complaints rather than treat a documented condition.
Move quickly on evidence preservation. Request medication administration records, physician orders, care plans, incident reports, and nursing notes, and compare them to the resident’s baseline behavior. Ask whether informed consent was obtained, whether non-drug interventions were attempted, and whether monitoring for side effects occurred. Document sudden sedation, falls, dehydration, or loss of mobility with timelines and witness statements from family, visitors, or roommates.
You strengthen your case with expert testimony from geriatric physicians, pharmacists, or nursing standards professionals who can explain proper indications, dosing, contraindications, and regulatory duties. If the facility ignored policies or falsified charts, you can clearly show negligence and causation.
Compensation for Fort Lauderdale Nursing Home Chemical Restraints Abuse Damages
Accountability often starts with compensation that reflects the harm chemical restraints caused your loved one. You can pursue damages for physical decline, falls, dehydration, pressure injuries, and medication side effects, plus emotional harm like fear, confusion, and loss of dignity.
You may also seek repayment of medical bills, added caregiving costs, and the value of services your family had to provide when the facility failed its duty.
To secure fair compensation, you’ll connect the drugging to measurable losses. A medical expert can explain how improper sedatives worsened mobility, cognition, or breathing, and why the facility’s records don’t match safe practice.
Your family testimony can show the day-to-day change in personality, engagement, and independence. During settlement negotiation, you can demand reforms, including a safer care plan, staffing oversight, and monitoring, so your claim serves your loved one and protects other residents, too.
The Statute of Limitations for Fort Lauderdale Nursing Home Chemical Restraint Abuse Cases
Pursuing damages only works if you file your claim on time, and Florida’s deadlines can move quickly in nursing home chemical restraints abuse cases. When you act promptly, you protect a vulnerable resident’s voice and help prevent future harm to others in care.
Florida’s statute limits depend on the legal theory you use, such as negligence, abuse, or wrongful death. You’ll also face specific nursing home presuit steps, which can shorten practical filing deadlines even when the calendar seems generous. Don’t wait for “one more record” or “one more conversation” if sedation, overmedication, or improper psychotropic use has caused injury.
Start by documenting when you first learned of the harm and when it happened, because discovery dates can affect the timeline. Preserve medication logs, care plans, incident reports, and witness notes now. If a resident died, the clock may run differently, so confirm the applicable deadline early.

Why You Need an Experienced Fort Lauderdale Nursing Home Chemical Restraints Abuse Lawyer
Even if the facility claims a medication was “for safety,” an experienced Fort Lauderdale nursing home chemical restraints abuse lawyer can spot the red flags, lock down vital records fast, and build a case that proves sedation crossed the line into unlawful restraint. You’re trying to protect someone who can’t always advocate for themselves, and you need a professional who understands how these cases hide in plain sight.
You’ll face chart notes that minimize side effects, vague “behavior” labels, and shifting explanations. A seasoned lawyer presses for complete MARs, nursing notes, care plans, and incident reports, then compares them to what should’ve happened.
They scrutinize Staffing Ratios to determine whether understaffing led to shortcuts, and they demand Medication Audits to uncover patterns of PRN overuse, dose stacking, or improper consent. You also get help identifying qualified medical experts, calculating harm, and stopping continued overmedication.
Your advocacy becomes evidence-backed action that secures accountability and safer care.
How to Choose the Right Fort Lauderdale Nursing Home Chemical Restraints Abuse Lawyer for Your Case
Because chemical restraint cases often look like routine “behavior management” on paper, you need a Fort Lauderdale lawyer who knows how to read between the lines and prove when medication became unlawful restraint.
Choose counsel who understands dosing patterns, PRN orders, charting gaps, and staffing pressures that can hide abuse.
Start by asking how they investigate: Do they obtain MARs, care plans, incident reports, and pharmacy records quickly? Do they work with geriatric and pharmacology experts? During client interviews, you should feel heard, not rushed, and you should get clear guidance on protecting your loved one while the case moves forward.
Evaluate communication and values: you want someone who treats the facility’s residents with dignity and keeps you updated. Finally, compare fee structures in writing, including costs, contingency terms, and what happens if the case doesn’t resolve.
Choose the lawyer who pairs skill with service-minded purpose.
About the Law Offices of Anidjar and Levine
Turn to the Law Offices of Anidjar and Levine when you need a Fort Lauderdale legal team that takes suspected nursing home chemical restraint abuse seriously and moves quickly to protect your loved one.
You’ll get steady guidance, clear options, and a plan focused on safety, dignity, and accountability.
You can lean on a team built to serve families in crisis. The Firm’s history reflects years of advocating for people harmed by neglect and misconduct, and you’ll see that commitment in how they communicate, investigate records, and press facilities to answer for drug misuse. You won’t be left guessing about next steps or timelines.
When you’re deciding who to trust, you can review Client testimonials that highlight responsiveness, compassion, and results-driven work.
You’ll also get help gathering medical charts, staffing logs, and incident reports while your loved one’s well-being stays the priority. You’ll feel supported from start to finish.
Frequently Asked Questions
What Is the Difference Between Chemical and Physical Restraints in Nursing Homes?
Chemical restraints use medications to control behavior or sedate you, often limiting your medication autonomy.
Physical restraints use devices or manual holds to restrict your movement, like belts, bed rails, or chairs.
You’ll notice chemical restraintsaffect alertness and mood, while physical restraints affect mobility and comfort.
You can advocate for dignity by asking care teams to document necessity, monitor effects, and prioritize restraint alternatives like calming routines, pain relief, and engagement.
Are Antipsychotics Ever Legally Prescribed for Dementia-Related Behaviors?
Yes, antipsychotics can be legally prescribed for certain dementia-related behaviors, but you must meet strict safeguards.
You need a documented clinical indication, a careful risk-benefit review, and informed consent from you or your surrogate when required.
You should try non-drug approaches first and use the least restrictive option at the lowest effective dose for the shortest time.
You must monitor closely and regularly reassess, tapering when possible.
Can I Access My Loved One’s Pharmacy Records Without Power of Attorney?
You usually can’t access your loved one’s pharmacy records without a power of attorney or a signed HIPAA authorization.
You can request proxy access if the pharmacy offers it, but they’ll still require documentation and may limit what you see.
If your loved one has capacity, ask them to sign a consent; if they later choose consent revocation, the pharmacy must stop sharing.
If capacity is impaired, pursue guardianship or consult counsel quickly.
Do Nursing Homes Have to Report Restraint Use to State or Federal Agencies?
Yes, nursing homes generally must document restraint use and may have to report certain incidents under state reporting rules and federal oversight.
You’ll see requirements tied to care plans, physician orders, and resident rights.
If restraints cause injury, improper sedation, or a significant change in condition, the facility often must notify regulators and the resident’s representative.
You can request records, ask about reporting policies, and escalate concerns to your state survey agency.
Will Filing a Claim Affect My Loved One’s Medicaid or Medicare Benefits?
Filing a claim usually won’t reduce your loved one’s Medicare benefits, and it typically won’t end Medicaid, but a settlement can affect Medicaid eligibility if it raises countable assets.
You’ll want asset protection planning and benefits counseling before you accept any payment or structure it. You can use special needs trusts or structured settlements in some cases. You should also report changes promptly to avoid overpayments.
———————–
You don’t have to face nursing home chemical restraint abuse alone in Fort Lauderdale.
If you suspect a loved one was improperly medicated to control their behavior, you can take action and demand answers. Start by documenting what you’ve observed, requesting detailed medical and medication records, and reporting the facility to the appropriate authorities when necessary.
An experienced Fort Lauderdale Nursing Home Abuse and Neglect Lawyer can investigate what happened, identify those responsible, and pursue compensation for the harm caused.
Contact the Law Offices of Anidjar and Levine today to discuss your legal options.