At the Law Offices of Anidjar and Levine, we handle Florida post-surgical infection cases by securing records, consulting infectious disease and surgical experts, and proving duty, breach, causation, and damages under Florida’s pre-suit rules.
We document timelines, sterilization and antibiotic protocols, and infection control lapses, then confront insurers with evidence-driven demands.
We quantify medical costs, lost income, and pain and suffering, negotiate liens, and pursue settlement, ADR, or trial within strict statute deadlines.
We manage communications and provide clear updates, and the following sections explain what to do next.
Learn more about how we can help: Medical Malpractice Injury Lawyer
Key Takeaways
- Florida attorneys investigate post-surgical infections by securing records, consulting experts, and proving duty, breach, causation, and damages under state medical malpractice law.
- They handle presuit screening and corroborating expert opinions, meeting Florida’s strict notice and statute-of-limitations requirements.
- Lawyers gather sterilization logs, operative notes, antibiotic orders, culture results, and infection-control records to establish breaches of the standard of care.
- Firms manage insurer and hospital communications, preserve evidence, and prepare cases for negotiation, settlement, or trial to maximize recovery.
- Consult early to protect deadlines, clarify timelines, quantify economic and non-economic losses, and align strategy with your goals on a contingency fee basis.
How We Can Help With Your Florida Post-Surgical Infection Injury Claim
You can direct your claim with a focused legal strategy built around evidence and accountability.
Dig deeper into our in-depth case study: Florida Post-surgical Infection Injury Lawyer
We begin by listening carefully, documenting your experience, and identifying every party responsible.
Our team secures medical records, consults qualified experts, and builds a clear causal narrative that supports liability and damages.
We obtain records, consult experts, and craft a persuasive causal narrative proving liability and damages.
We center patient advocacy in every step, ensuring your voice is heard and your needs guide our priorities.
We manage communications with insurers and providers to prevent misstatements and preserve your rights.
Our valuation process is disciplined, incorporating medical costs, lost income, and long-term impacts.
We prepare each case as if for trial, which strengthens our position during settlement negotiations and promotes fair outcomes.
When appropriate, we pursue alternative dispute resolution to expedite relief without compromising value.
Throughout the process, we provide timely updates, practical guidance, and decisive representation.
Our goal is straightforward: to protect you, efficiently advance your claim, and obtain the compensation necessary for recovery.
Understanding Florida Post-surgical Infection Injury Cases
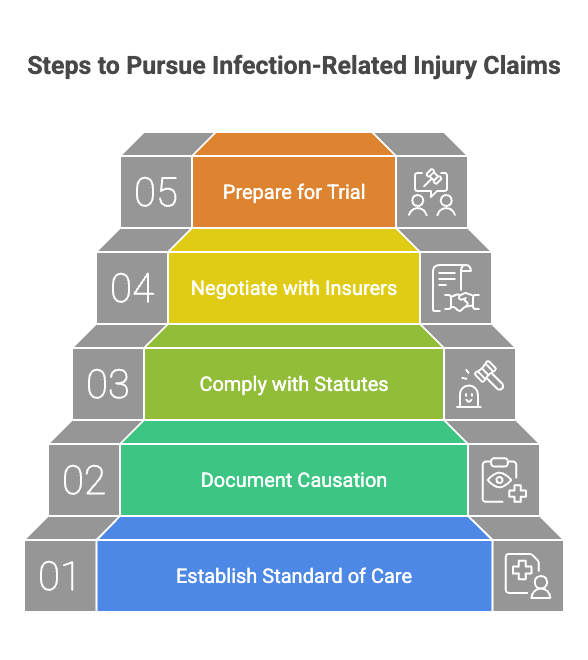
With your claim strategy underway, we should understand how Florida law frames post-surgical infection injuries and what must be proven. To establish liability, we must show a duty of care, a breach of accepted medical standards, causation linking that breach to the infection, and measurable damages.
Medical records, expert testimony, and infection timelines will be central, as will proof of adherence to physician orders.
Florida’s presuit screening requirements apply, demanding corroborating expert opinions before filing. We also evaluate compliance with hospital protocols, informed consent disclosures, and the adequacy of patient education regarding symptoms, wound care, and follow-up.
Documentation of post-discharge monitoring, such as telehealth check-ins and prompt cultures, can either support or undermine defenses.
Damages include medical costs, lost income, pain and suffering, and, in severe cases, long-term disability. The statute of limitations is strict, with potential tolling for delayed discovery. We prepare evidence early, preserve witnesses, and coordinate expert reviews to protect your rights.
Common Causes of Florida Post-surgical Infection Injuries
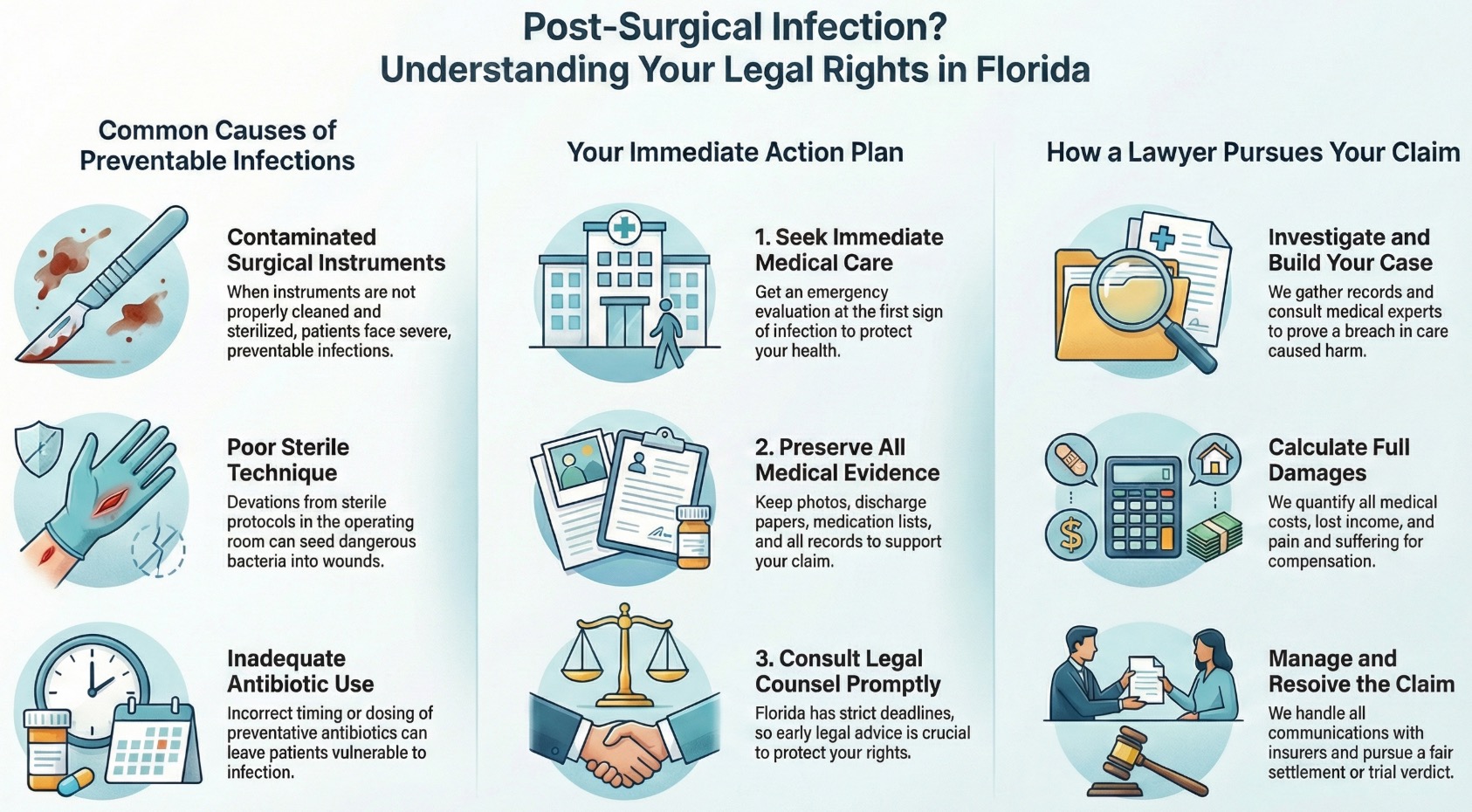
As we examine what causes post-surgical infection injuries in Florida, we often find contaminated surgical instruments and poor sterile technique at the forefront.
We also see preventable failures, such as inadequate antibiotic prophylaxis, which can leave patients vulnerable during crucial windows.
Compounding these risks, hospital-acquired resistant bacteria can turn a manageable infection into a severe, prolonged injury.
Contaminated Surgical Instruments
Contamination is a preventable breach that turns routine surgery into a serious health risk. When instruments aren’t properly cleaned and sterilized, patients can face severe infections, extended hospitalizations, and lasting harm.
We focus on proving where the chain of safety failed, emphasizing rigorous instrument sterilization and proper handling before every procedure.
Hospitals must follow strict protocols for decontamination, packaging, storage, and surgical tray validation to ensure that every instrument meets sterility parameters. Breakdowns in tracking, maintenance, or post-sterilization handling can introduce pathogens, even when systems appear compliant.
We investigate logs, cycle records, and vendor standards to identify deviations and accountability.
If contaminated surgical instruments led to a postoperative infection, we’re prepared to act. We gather evidence swiftly, consult qualified experts, and pursue compensation that supports recovery and safeguards others.
Poor Sterile Technique
Often overlooked but entirely preventable, poor sterile technique can seed dangerous bacteria into a surgical field and trigger a post-operative infection. When operating room teams deviate from established protocols, patients bear the risk.
We examine glove integrity, hand antisepsis, gowning and draping, and adherence to sterile zones, because minor aseptic breaches can have outsized consequences. Breaks in laminar flow, unnecessary traffic, or incorrect instrument handling allow contaminants to settle into wounds.
We work to identify who touched what, when barriers were compromised, and whether counts, timing, and field maintenance met standards. Video, staffing logs, and environmental records reveal systemic gaps.
By tracing each step, we hold facilities and clinicians accountable, drive corrective practices, and seek compensation that supports recovery while promoting safer care for future patients.
Inadequate Antibiotic Prophylaxis
Breaks in sterile technique aren’t the only pathway to harm; failures in antibiotic prophylaxis also set the stage for post-surgical infections. When providers miss the crucial window for antibiotic timing, protective levels aren’t present when contamination risk peaks.
Dosing errors further compound risk, especially for patients with obesity, renal impairment, or lengthy procedures, where standard doses don’t achieve adequate tissue concentrations.
We examine orders, anesthesia records, and nursing charts to confirm that selection, timing, and redosing aligned with established guidelines. We also assess documentation of allergies and contraindications, because improper substitutions can render prophylaxis ineffective.
If protocols were ignored or applied inconsistently, we would build a precise record of causation and damages.
Our aim is straightforward: hold negligent actors accountable and secure resources for your recovery.
Hospital-Acquired Resistant Bacteria
Confront the reality that hospitals can harbor drug‑resistant organisms—MRSA, VRE, ESBL‑producing gram‑negatives, and carbapenem‑resistant strains—that complicate even routine postoperative care.
These pathogens spread through lapses in hand hygiene, inadequate device protocols, and delayed isolation, placing vulnerable surgical patients at risk. We recognize how swiftly a minor wound issue can become a life‑altering infection.
We evaluate whether facilities implemented antibiotic stewardship to minimize unnecessary broad‑spectrum use, and whether resistance surveillance identified emerging threats in the unit. We examine culture timing, source control, and appropriate empiric therapy, then measure responses against accepted standards.
When hospitals fail to monitor resistance patterns, clean environments, or enforce contact precautions, patients suffer preventable harm. We stand ready to investigate, preserve evidence, and hold facilities accountable for avoidable, hospital‑acquired resistant infections.
Legal Rights of Florida Post-surgical Infection Injury Victims
While a post-surgical infection can upend recovery, Florida law affords clear rights to seek accountability and compensation when negligence plays a role. We’ve a legal framework that recognizes breaches in sterile technique, poor monitoring, and delayed diagnosis as actionable medical negligence.
Our role is to protect your interests, advance patient advocacy, and guarantee your claim reflects the full scope of harm, including additional care, wage loss, and long-term effects.
- You’re entitled to pursue damages when providers deviate from the accepted standard of care, supported by expert testimony and documented causation.
- Florida’s statutes govern deadlines, pre-suit investigations, and notice requirements, which we strive to preserve claims and leverage compliance failures.
- We confront insurance disputes with evidence-driven negotiation and prepare for trial when carriers undervalue infection-related injuries.
We seek accountability from all responsible parties, including hospitals, surgeons, and contractors. By asserting your rights with precise documentation and credible experts, we help secure compensation that supports recovery, restores dignity, and safeguards future care.
Steps to Take After a Florida Post-surgical Infection Injury
After a post-surgical infection, we should act promptly by seeking immediate medical care to stabilize health and document symptoms.
We must preserve medical evidence, including photographs of the wound, medication lists, discharge instructions, and follow-up records, to support both treatment and potential claims.
We should then consult legal counsel without delay, ensuring deadlines are met, and evidence is evaluated to protect our rights.
Seek Immediate Medical Care
Recognizing a potential post-surgical infection and acting without delay protects your health and preserves essential evidence. If you notice fever, escalating pain, redness, warmth, foul drainage, or swelling, seek an emergency evaluation immediately.
Rapid treatment can prevent worsening complications, limit tissue damage, and support a safer recovery. We would like to encourage you to contact your surgeon or visit the nearest emergency department as soon as symptoms arise.
During medical care, request a focused wound assessment and precise documentation of findings, including critical signs, lab orders, and prescribed antibiotics. Provide a complete symptom timeline, medication list, and any allergies.
Follow discharge instructions exactly, and schedule prompt follow-up with your surgeon or primary physician. If transportation or communication is a barrier, ask for assistance. Timely, decisive action safeguards your well-being.
Preserve Medical Evidence
Building a clear medical record from the outset strengthens your claim and helps establish causation and damages. We should take care of all relevant medical evidence as soon as possible. Save operative reports, nursing notes, discharge instructions, medication lists, and wound photographs with timestamps.
Request copies of culture results, imaging, and laboratory values, including microbiology testing that identifies organism type and antibiotic sensitivities. Maintain original packaging for prescribed devices or dressings when feasible.
We must also protect the integrity of physical evidence. Store wound swabs or removed hardware as directed by medical professionals, and document a transparent chain of custody for any specimens or items retained.
Keep a treatment journal noting symptoms, fevers, antibiotics, and follow-up appointments. Organize records chronologically, verify accuracy, and promptly correct discrepancies in provider portals.
Consult Legal Counsel
Even as we stabilize your health and document the infection, consulting experienced legal counsel early is crucial to protect your rights and maximize your recovery. When we engage promptly, we preserve evidence, secure expert reviews, and comply with Florida’s strict deadlines. We begin with thorough client interviews to clarify your medical timeline, providers involved, and damages, then identify potential negligence and causation issues.
We explain fee structures transparently, including contingency arrangements, expert costs, and how expenses are advanced and reconciled. Early counsel also coordinates communications with insurers and hospitals, preventing misstatements and protecting privileged information.
We obtain records, evaluate liability and coverage, and develop a litigation or settlement strategy aligned with your goals. By acting now, we position your claim for a timely, well-supported, and just result.
How a Florida Post-surgical Infection Injury Lawyer Can Help You
While the medical focus remains on healing, a Florida post-surgical infection injury lawyer steps in to protect your legal and financial recovery. We gather medical records, consult authorities, and pinpoint breaches in standards of care. We coordinate with your providers, calculate damages with precision, and negotiate firmly with insurers. Our role is to shoulder the legal burden so you can focus on health and service to your loved ones.
We also strengthen your voice through clear patient education, ensuring you understand your rights, options, and timelines. When needed, we connect you with vetted support groups, community resources, and practical tools to sustain resilience throughout the claims process.
- Case building: obtain records, preserve evidence, and retain credentialed experts to analyze causation and liability.
- Damages strategy: quantify lost wages, additional treatment costs, and non-economic harm, backed by documentation.
- Resolution path: pursue settlement where appropriate, prepare litigation when necessary, and keep you informed at each step.

Long-term Effects of Florida Post-surgical Infection Injuries
We should address how post-surgical infections can lead to chronic pain and scarring that persist long after the initial procedure, often complicating recovery and daily comfort.
We’ll also examine mobility and functional loss, including reduced range of motion and weakness, which may require extended therapy or adaptive support.
Finally, we’ll consider the emotional and financial strain, from anxiety and depression to mounting medical bills and lost income, and how these burdens shape long-term outcomes.
Chronic Pain and Scarring
Living with chronic pain and visible scarring after a post-surgical infection can reshape daily life, mobility, and self-image. We recognize how persistent pain erodes stamina, sleep, and focus, especially when nerve entrapment develops within inflamed or fibrotic tissue.
Some clients experience burning or stabbing sensations that fluctuate, yet never fully remit, demanding careful documentation and targeted medical care.
Scarring also brings distinct burdens. Keloid formation may extend beyond the incision, thicken over time, and cause itching, tenderness, and hypersensitivity. These changes can limit clothing choices, complicate hygiene, and undermine confidence in public or professional settings.
We work to connect you with medical experts, preserve medical evidence, and advocate for treatments and compensation that address pain management, scar revision, and long-term supportive care.
Mobility and Function Loss
Although recovery from surgery should restore strength and motion, a post-surgical infection can instead trigger lasting loss of mobility and function that alters how you move, work, and care for yourself. When infection damages tissue, joints, or nerves, the range of motion declines, gait becomes unstable, and daily tasks require greater effort.
We often see reduced endurance, stiffness, and weakness that complicate lifting, bending, or standing.
With timely intervention, we can stabilize function and promote independence. Targeted rehabilitation, including adaptive therapy, addresses strength, balance, and coordination. Physicians may recommend bracing, orthotics, or other assistive devices to protect healing structures and support safe movement.
We coordinate expert evaluations, document limitations with precision, and pursue resources for durable equipment and ongoing therapy, helping you regain safe, sustainable mobility.
Emotional and Financial Strain
Uncertainty compounds the toll of a post-surgical infection, as mounting medical needs collide with disrupted income and rising household pressures. We see families stretch savings, delay bills, and make difficult choices about care, all while trying to support healing.
The emotional cost is equally weighty. Anxiety, sleep disruption, and fear of complications strain mental health, and caregivers often shoulder quiet burdens that erode resilience.
We help you map a path forward, prioritizing treatment continuity, access to counseling, and practical supports. Documenting lost wages, out-of-pocket costs, and home-care expenditures positions us to pursue thorough financial recovery.
We assess insurance gaps, negotiate medical liens, and seek damages for future care. With disciplined planning and assertive advocacy, we work to stabilize today’s needs and protect tomorrow’s security.
Proving Liability in Florida Post-surgical Infection Medical Malpractice Injury Cases
When a post-surgical infection occurs, proving liability in Florida hinges on demonstrating that a provider breached the applicable standard of care and that this breach caused the infection and resulting damages.
We begin by gathering operative notes, nursing records, and infection control logs, then compare those actions to accepted protocols for sterilization, antibiotic prophylaxis, wound care, and timely recognition of symptoms.
We evaluate whether informed consent addressed known infection risks and alternatives, because inadequate disclosures can support liability where consent was deficient.
We rely on expert testimony from qualified surgeons, nurses, and infectious disease authorities to establish what a reasonably prudent provider would have done, and to link deviations to the infection.
We also secure cultures, lab results, and timelines that show when contamination likely occurred.
Witness statements and facility policies help confirm systemic lapses.
Compensation for Florida Post-surgical Infection Damages
Compensation in Florida post-surgical infection cases aims to make you whole by addressing both immediate losses and long-term consequences. We pursue damages that reflect the full scope of harm, beginning with medical costs for hospitalization, revision procedures, wound care, medications, and rehabilitative services.
Compensation addresses immediate losses and long-term consequences, from medical costs to comprehensive rehabilitative services.
We also seek compensation for lost income and diminished earning capacity when recovery disrupts employment or limits future opportunities.
Pain and suffering damages account for physical pain, daily limitations, and the strain on family life. We document the impact through medical records, expert evaluations, and your own account of functional changes.
Emotional recovery matters as well, so we include damages for anxiety, depression, sleep disruption, and loss of enjoyment of life linked to the infection and treatment.
When complications lead to scarring, disability, or the need for assistive devices, we quantify their lasting effects.
Finally, we address out-of-pocket expenses, including travel, home modifications, and necessary caregiving support.
The Statute of Limitations for Florida Post-surgical Infection Injury Cases
Although the aftermath of a post-surgical infection can be overwhelming, we must act quickly because Florida imposes strict deadlines for filing injury claims. The Statute limits control when a case may be brought, and missing a deadline can forfeit the right to recover.
In medical negligence matters, the general Filing deadlines are two years from when the injury is discovered, or should have been discovered with reasonable diligence, and no later than four years from the date of the negligent act, subject to limited exceptions.
We should also consider tolling rules, which may extend time in cases of fraud, concealment, or when the injured person is a minor. Pre-suit investigation and notice requirements consume precious time, so early evaluation is crucial. Preserving medical records, infection logs, and correspondence supports timely compliance.
When we act promptly, we safeguard evidence, meet statutory notice obligations, and align our efforts with Florida’s Statute limits, protecting the claim’s viability and the community we aim to serve.
Why You Need an Experienced Florida Post-surgical Infection Injury Lawyer
Because post-surgical infection cases hinge on complex medical facts and strict procedural rules, we need an experienced Florida attorney to navigate the terrain with precision. An experienced lawyer interprets operative reports, cultures, and timelines, aligning them with Florida standards of care.
We rely on this skill to prove causation, quantify damages, and preserve claims under demanding deadlines.
We also need rigorous patient advocacy that centers on your recovery and long-term needs. A seasoned attorney coordinates expert testimony, analyzes hospital protocols, and identifies systemic failures that contributed to harm.
This disciplined approach helps us present a straightforward narrative to insurers, defense counsel, and, when necessary, a jury.
Strong settlement negotiation is vital because insurers often minimize infection-related losses. With proven valuation methods and strategic leverage, an experienced lawyer pursues compensation for medical expenses, wage disruption, and future care.
If fair resolution isn’t offered, we’re prepared to litigate decisively, safeguard evidence, and advance your case with unwavering focus.
How to Choose the Right Florida Post-surgical Infection Injury Lawyer for Your Case
Start by evaluating credentials that directly align with post-surgical infection litigation, then verify results and resources. We should confirm board certifications, trial experience, and a track record in hospital-acquired infection cases. Case outcomes, published verdicts, and peer recognition help us gauge reliability.
We also assess whether the firm has medical experts, investigative capacity, and litigation technology to handle intricate causation and damages.
Next, we conduct focused client interviews to understand approach and communication style. We ask how the attorney builds timelines, preserves evidence, and negotiates with insurers and hospitals.
Clarity in Fee structures is vital; we seek written contingency terms, cost-advancement policies, and transparency regarding expert fees and potential liens.
We evaluate responsiveness and reporting cadence to ensure regular updates and clear next steps. Finally, we confirm conflict checks, ethical standing, and willingness to proceed to trial if necessary. With these measures, we choose counsel equipped to protect your interests.
About the Law Offices of Anidjar and Levine
Built on responsive advocacy and disciplined litigation, the Law Offices of Anidjar and Levine focuses on delivering thorough representation to patients harmed by post-surgical infections across Florida.
We approach each case with meticulous preparation, clear communication, and unwavering accountability, because your recovery and dignity matter.
Our team coordinates investigations, consults medical experts, and pursues liable parties, while keeping you informed at every step.
Our firm’s history reflects a sustained commitment to injured clients and communities statewide. We’ve grown by serving with integrity, improving our processes, and investing in technology that strengthens evidence collection and case management.
Client testimonials consistently highlight our responsiveness, professionalism, and results, validating our mission to combine compassion with rigorous advocacy.
We collaborate with healthcare consultants to document standards of care, causation, and damages, and we structure strategies around your unique medical needs.
We’re prepared for negotiation or trial, and we prioritize timely action to protect your rights and maximize your recovery.
Frequently Asked Questions
What Medical Records Should I Collect to Document My Infection’s Progression?
You should gather complete operative notes, discharge summaries, progress notes, nursing charts, and all laboratory reports, including cultures, sensitivities, CBCs, and inflammatory markers.
Let’s also include imaging studies, medication administration records, antimicrobial timing, and dosage details.
We should obtain wound care documentation, photos, temperature logs, and sepsis screens.
Collect consultation notes from infectious disease and surgery, plus follow-up visit records.
Finally, secure timelines of symptom onset, readmissions, and any adverse event reports.
Can I Pursue a Claim if I Signed Surgery Consent Forms?
Yes, you can still pursue a claim. Signing informed consent acknowledges known risks, but it doesn’t excuse negligent care, improper sterilization, or delayed diagnosis.
We’d assess whether providers met the standard of care and whether undisclosed risks or protocol breaches caused harm. Comparative negligence may reduce recovery if your actions contributed, but it doesn’t bar the claim. We’ll analyze records, expert opinions, and timelines to determine liability, causation, and the full measure of damages.
How Do I Preserve Infected Device or Implant Evidence?
Preserve the device by instructing the hospital, in writing, not to discard or alter it, and request sterile removal and sealed storage.
We document the chain of custody from the operating room to secure evidence storage, identifying each custodian.
We photograph implants immediately, including packaging, labels, and lot numbers.
We obtain pathology and microbiology reports, then secure independent testing.
Don’t handle the device yourself; we coordinate transport to an accredited lab under strict evidence protocols.
Will Reporting the Infection Affect My Ongoing Medical Care?
Yes, reporting the infection should improve, not jeopardize, your care. We notify surgeon teams promptly so they can adjust antibiotics, evaluate the wound, and coordinate timely interventions.
We document symptoms—onset, fever, drainage, redness, and pain—and share photos to ensure accurate assessment. We also request cultures and clarify follow‑up intervals, safeguarding continuity.
Transparent communication supports patient safety, reduces complications, and preserves treatment options, while creating a reliable record that guides decisions and demonstrates responsible, proactive care.
Can Telehealth Follow-Ups Impact Proving Post-Surgical Negligence?
Yes, telehealth follow-ups can affect the ability to prove post-surgical negligence. They create records, yet telemedicine limitations and reduced physical assessment may weaken proof compared to in-person care.
Virtual examinations can miss wound characteristics, odor, or subtle edema, complicating causation and timing. We recommend supplementing telehealth with prompt in-person evaluations, high-resolution photos, and temperature logs.
We’ll secure complete records, clarify decision-making, and consult experts to link symptoms, delays, and breaches of standard of care with precision and credibility.
——————————
We’re ready to protect your rights and pursue the compensation you deserve after a post-surgical infection.
We’ll investigate liability, secure expert testimony, and manage deadlines while you focus on recovery.
Our team evaluates damages, preserves evidence, and negotiates aggressively, preparing for trial when needed.
Don’t wait, as Florida’s statute of limitations can bar claims.
Contact the Law Offices of Anidjar & Levine for a free consultation.
We’ll provide clear guidance, dedicated advocacy, and relentless representation from start to finish.
Learn more here: Medical Malpractice Injury Lawyer