1.0 Introduction: The Critical Landscape of Medical Malpractice and Brain Injury
Brain injuries resulting from medical malpractice inflict profound and often permanent consequences on patients and their families, altering lives in an instant. Navigating the aftermath requires a deep understanding of the intricate legal and medical challenges involved.
Learn More: Florida Brain Damage Malpractice Injury Lawyer
For families in Florida, developing a sound strategy from the outset is not just beneficial—it is essential for securing the accountability and long-term resources necessary for a dignified future.
This analysis outlines the core components of a successful brain injury malpractice claim, from the initial preservation of evidence to the final pursuit of compensation. The key strategic considerations include:
- Proving Negligence: A successful claim hinges on the ability to demonstrate, through expert testimony and meticulous record review, that a healthcare provider deviated from the accepted standard of care.
- Time-Sensitivity: The legal process is governed by strict deadlines. Florida’s two-year statute of limitations and mandatory presuit notice requirements make early investigation and prompt action absolutely critical.
- Evidence Preservation: The immediate need to secure complete medical records—including audit trails, imaging files, anesthesia/device logs, and staffing records—cannot be overstated. This evidence is fundamental to building a precise timeline of events.
- Establishing Causation: The legal team must definitively link the medical error to the neurological injury. This is achieved through a combination of advanced neuroimaging, neuropsychological testing, and the analysis of independent medical experts.
- Documenting Future Needs: A comprehensive life-care plan is essential for quantifying the full scope of damages, including all future costs for therapies, assistive technology, supervision, and medical care.
These elements form the strategic framework for pursuing justice. We will now examine the foundational legal principles that govern these complex cases.
2.0 The Foundational Pillars: Standard of Care and Causation
To build a successful medical malpractice claim for a brain injury, one must first master two foundational legal concepts: the “standard of care” and “causation.” A case cannot proceed without establishing both with precision and irrefutable evidence. Defining these terms is the strategic core of any claim, transforming a suspicion of wrongdoing into a defensible case for liability.
2.1 Defining the Standard of Care
The accepted “standard of care” in Florida is the level of care, skill, and treatment that a reasonably prudent healthcare provider would have administered under similar circumstances. Our strategic assessment begins by benchmarking the provider’s actions against this standard. We analyze key decision points—including diagnostic choices, the timing of treatment, and discharge planning—to identify critical failures. A deviation from this standard, whether an act or an omission, constitutes a breach of the provider’s duty to the patient and is the first pillar in establishing negligence.
2.2 Proving Causation
Establishing a breach of care is only half the battle; the next step is to prove causation—that is, to draw a direct line from the provider’s failure to the specific neurological harm suffered. This requires a methodical, evidence-based approach that leaves no room for speculation. The following evidentiary tools are essential:
- Clinical Records and Timelines: A minute-by-minute reconstruction of events using medical charts, triage notes, and audit trails can reveal critical delays or errors that align directly with the onset of injury.
- Neuroimaging Advances: Detailed imaging, such as MRIs and CT scans, provides objective proof of the injury’s scope and nature, helping to distinguish new, malpractice-related damage from any preexisting conditions.
- Neuropsychological Testing: These evaluations provide a comprehensive assessment of functional deficits in cognition, language, behavior, and memory, creating a measurable record of the harm.
- Independent Expert Opinions: Qualified medical experts are indispensable for interpreting complex clinical data, explaining how the breach of care led to the injury, and refuting alternative explanations proposed by the defense.
Having established this theoretical framework, we can now turn to the common, real-world scenarios where these principles are most frequently applied.
3.0 Anatomy of a Malpractice Event: Common Causes of Brain Injury
While medical malpractice can manifest in countless ways, a few recurring scenarios are frequently identified as the root cause of preventable brain injuries. Understanding the mechanisms of these common errors is key to deconstructing the event, proving a breach of care, and establishing clear lines of liability.
3.1 Surgical Errors and Complications
Surgical procedures, though routine, carry inherent risks that are magnified by human error or systemic failures. Preventable brain injuries in the operating room often stem from:
- How it Occurs: Anesthesia mistakes that deprive the brain of oxygen (hypoxia), uncontrolled bleeding that goes unrecognized, or improper patient positioning that impairs circulation.
- Why it Breaches Care: Failures to follow established safety protocols, such as surgical checklists, can lead to wrong-site procedures, medication mix-ups, or retained instruments. Lapses in sterile technique may cause severe infections that affect the brain.
- Proof of Liability: Liability is established by meticulously analyzing anesthesia records, device logs, and staffing assignments to reconstruct the timeline of the event. Expert testimony is used to confirm that the team deviated from accepted surgical protocols and that this deviation directly caused the harm.
3.2 Misdiagnosis or Delayed Diagnosis
Time is a critical factor in treating conditions that can cause brain damage. A failure to act promptly can turn a treatable condition into a permanent injury.
- How it Occurs: Clinicians fail to recognize the signs of a stroke, hemorrhage, infection, or hypoxia, leading to a critical delay in treatment.
- Why it Breaches Care: The standard of care requires providers to order appropriate diagnostic tests promptly, interpret the results accurately, and escalate care or seek a specialty consultation without delay. A failure to do so is a clear breach.
- Proof of Liability: Evidence is built by examining triage notes, lab and imaging results, and transfer decisions. A precise timeline is constructed to demonstrate how delays in diagnosis and treatment correspond directly to the progression of the neurological damage.
3.3 Anesthesia Monitoring Failures
Continuous and vigilant monitoring is the cornerstone of safe anesthesia administration. A moment of inattentiveness can have catastrophic consequences.
- How it Occurs: Anesthesia teams fail to continuously track and respond to vital signs, including oxygenation (pulse oximetry), ventilation (capnography), circulation (blood pressure), and depth of anesthesia. Breakdowns in monitoring protocols, poor handoffs between staff, or simple inattentiveness can precede a severe hypoxic event.
- Why it Breaches Care: The standard of care demands that clinicians respond to monitor alarms or shifting trends within seconds, not minutes. Any lapse in this vigilance is a direct breach of duty.
- Proof of Liability: Anesthesia records, electronic device logs, and staffing assignments are secured to reconstruct the event. Anesthesiology experts are consulted to identify the precise moment of deviation and confirm that it was the cause of the oxygen deprivation and subsequent brain injury.
3.4 Medication Dosing Mistakes
The administration of powerful medications requires absolute precision. Miscalculations or systemic failures in the medication-use process can cause severe, irreversible brain damage.
- How it Occurs: A provider miscalculates a dose of a sedative, anticoagulant, insulin, or vasoactive drug, leading to hypoxia, hemorrhage, or ischemia (inadequate blood supply).
- Why it Breaches Care: Systemic failures—such as poor pharmacy oversight, absent double-checks for high-alert medications, or communication gaps during handoffs—violate established safety protocols.
- Proof of Liability: Pharmacy records, infusion pump logs, and electronic order entries are analyzed to pinpoint where the protocol broke down. Evidence of barcode mismatches, look-alike vials, overridden warnings, or failures to make weight-based adjustments often signal systemic negligence for which the facility is liable.
Understanding the cause of the injury is the first step; the next is to take immediate, practical action in response.
4.0 The Critical First Response: A Protocol for Suspected Malpractice
In the hours and days following a suspected medical malpractice event, the situation is often chaotic and emotionally overwhelming. However, the actions taken during this critical window can profoundly impact both the patient’s long-term health and the viability of any future legal claim. A disciplined, three-step protocol is essential.
1. Seek Immediate Medical Care The first priority is always the patient’s health. Prompt evaluation is critical to stabilize the patient’s condition, prevent secondary harm, and create an accurate clinical record of their status immediately following the suspected event. This involves calling 911 if symptoms like confusion, severe headache, or seizures appear. At the hospital, families should advocate for clear triage, provide a concise history of symptoms, and request neurology involvement when appropriate. Swift medical intervention not only supports recovery but also lays a sound evidentiary foundation for the case.
2. Preserve All Evidence and Records While focusing on medical care, it is equally important to begin preserving every piece of information related to the event. This evidence will be crucial for proving what happened and why. A comprehensive preservation strategy includes:
- Requesting complete medical charts, medication logs, imaging, and electronic audit trails in writing.
- Saving all appointment reminders, discharge instructions, and billing statements.
- Securing clear photos of injuries as they evolve.
- Preserving any relevant medical devices, packaging, and labels, maintaining a clear chain of custody.
- Identifying and storing the names, roles, and contact information of any potential witnesses.
- Requesting copies of any facility incident reports related to the event.
- Preserving all voicemail, text, and email communications with providers.
- Keeping a detailed journal documenting symptoms, treatments, and conversations.
3. Consult an Experienced Attorney Contacting a seasoned medical malpractice attorney as early as possible is a critical strategic move. An experienced lawyer can immediately take steps to formally preserve evidence, evaluate potential liability, and ensure all unforgiving legal deadlines are protected. Early consultation reduces the risk of costly missteps and positions the claim for maximum leverage from the very beginning.
This initial response protocol sets the stage for the formal legal process of establishing liability, which is the lawyer’s primary role in managing the case.
5.0 Proving Liability: The Strategic Legal Process in Action
Formally establishing legal liability is a methodical, evidence-driven process that moves beyond suspicion to build a compelling and defensible narrative of negligence and harm. This process is designed to hold the responsible parties accountable and secure the resources needed for the victim’s recovery.
5.1 Case Investigation and Proof Development
The legal process begins with a deep-dive investigation. The legal team’s first step is to secure all relevant medical records, including electronic charts and audit trails, to reconstruct a precise timeline of events. Concurrently, they consult with highly qualified medical experts in the relevant specialties (e.g., neurology, surgery, anesthesiology) to define the applicable standard of care. By comparing the provider’s actions to this standard within the context of the timeline, the team can pinpoint the exact breach of duty that led to the injury.
5.2 Expert Testimony
Expert witnesses play an indispensable role in a medical malpractice case. Their testimony serves several critical functions:
- Define the Breach: They explain to a judge or jury what the standard of care was and how the defendant’s actions fell short.
- Anchor the Causation Analysis: They connect the medical error directly to the brain injury, explaining the biological mechanisms of the harm (e.g., how a lack of oxygen led to cell death).
- Address Alternative Explanations: They systematically evaluate and refute other potential causes for the injury, isolating the provider’s negligence as the primary factor.
- Confirm Foreseeability: They confirm that the harm suffered was a predictable result of the medical error, a key element in proving legal negligence.
5.3 Insurance Negotiation and Litigation Readiness
The vast majority of malpractice cases are resolved through settlement, not a trial. However, the strongest negotiating position comes from preparing every case as if it will go to trial. This dual strategy involves methodically building a powerful, evidence-based case while simultaneously engaging with the provider’s insurance company. By presenting clear proof of liability and well-documented damages, the legal team creates significant leverage. This approach pressures insurers to offer fair compensation, as the alternative is facing a well-prepared and determined legal team in court.
Once liability is firmly established, the focus shifts to the crucial task of defining and quantifying the full extent of the damages.
6.0 Quantifying the Impact: Documenting Damages and Long-Term Needs
The ultimate goal of a malpractice claim is to translate the devastating human consequences of a brain injury into a comprehensive and legally defensible claim for compensation. This is not about assigning a dollar value to a life, but about securing the financial resources required to sustain dignity, provide necessary care, and ensure stability for a lifetime.
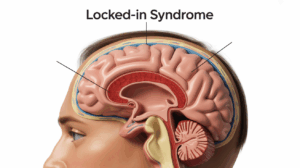
6.1 The Long-Term Effects of Brain Injury
A brain injury’s impact extends far beyond the initial medical crisis, often resulting in lifelong challenges that must be fully documented.
- Cognitive and Memory Decline: Patients frequently suffer from deficits in short-term memory, making it difficult to learn new information. They may also experience language impairment (e.g., slowed word-finding) or visuospatial decline, which complicates navigation and mobility.
- Emotional and Behavioral Changes: It is common to see significant shifts in personality, including pronounced mood swings, irritability, anxiety, and depression. These changes can strain family relationships and require specialized therapeutic support.
- Lifelong Care and Costs: A severe brain injury often necessitates ongoing neurologic care, extensive therapies (physical, occupational, speech), significant home modifications (ramps, roll-in showers), and assistive technology (communication devices, mobility aids).
6.2 Translating Harm into Compensation
Under Florida law, victims of medical malpractice are entitled to seek compensation for the full range of their losses. These damages are typically categorized as follows:
| Damage Category | Description |
| Economic Damages | Covers projected lifetime medical expenses, in-home assistance, rehabilitation, lost earnings, and diminished earning capacity. These are documented by life-care planners and economists. |
| Non-Economic Damages | Compensation for pain, suffering, loss of enjoyment of life, and the impact on family relationships (loss of consortium). |
| Punitive Damages | May be sought in rare cases involving intentional misrepresentation, fraud, or other egregious conduct that rises to a higher legal standard under Florida statutes. |
6.3 Protecting Financial Recovery
Securing a settlement or verdict is only part of the process. A comprehensive strategy must also include protecting the financial recovery itself. This involves carefully coordinating existing health insurance coverage, satisfying any medical liens, and engaging in special needs planning. For example, structuring the recovery properly and managing applications for benefits like Medicaid or SSI can preserve eligibility for essential government programs, maximizing the net resources available to the family for long-term care.
This detailed accounting of harm provides the substance of the claim, which must then be advanced according to the strict procedural rules of Florida’s legal system.
7.0 Navigating Florida’s Legal System: Timelines, Procedures, and Representation
Even the most compelling, well-documented medical malpractice case can fail if the strict procedural rules of the Florida legal system are not followed to the letter. Navigating this complex landscape requires diligence, expertise, and a keen awareness of the unforgiving deadlines that govern every claim.
7.1 The Florida Statute of Limitations
In medical malpractice cases, time is of the essence. Florida law imposes strict deadlines for filing a claim, and missing them can permanently bar a victim’s right to seek compensation.
- Statute of Limitations: A claim must generally be filed within a two-year period from the time the malpractice was discovered or reasonably should have been discovered.
- Statute of Repose: There is also a four-year absolute deadline from the date the incident occurred, which bars most claims filed after that time, regardless of when the injury was discovered.
- Tolling: The filing of a required presuit notice can temporarily “toll” or pause the statute of limitations for a limited time. In rare cases involving fraud or concealment by the provider, the deadline may also be extended.
7.2 The Importance of Experienced Counsel
A brain injury claim is not a matter for a general practice attorney. It demands counsel with a deep understanding of both complex medicine and unforgiving legal procedure. An experienced lawyer brings disciplined analysis to medical records, has access to a network of credible experts, and knows how to translate complicated medical findings into persuasive evidence. This experience is vital for countering the tactics of insurance companies, who will relentlessly challenge liability, causation, and the valuation of damages at every turn.
7.3 Criteria for Selecting Your Legal Advocate
Choosing the right legal representation is one of the most important decisions a family will make. The selection process should be guided by clear, objective criteria to ensure the chosen firm has the requisite skill and resources.
- Verify trial experience specifically in complex medical negligence and brain injury cases.
- Review representative settlements and verdicts to assess the firm’s track record of results.
- Evaluate the attorney’s command of medicine, case valuation methods, and communication style during the initial consultation.
- Compare fee structures in writing, ensuring you understand contingency percentages and how case costs are handled.
- Confirm the firm has ready access to essential resources, including top-tier neurologists, life-care planners, and economists.
Following this structured approach ensures that your case is managed with the diligence and expertise required to navigate Florida’s challenging legal environment, which is the final key to success.
8.0 Conclusion: Securing Accountability and a Path Forward
The strategic management of a brain injury medical malpractice claim in Florida is a complex undertaking that demands a combination of legal acumen, medical knowledge, and unwavering advocacy. It requires a methodical approach that begins with a rapid response and rigorous evidence preservation, builds upon the foundational pillars of standard of care and causation, and culminates in a meticulously documented case for full and fair compensation.
Success ultimately depends on three key factors: immediate action to protect both the patient’s health and legal rights, rigorous evidence preservation to build an irrefutable case, and seasoned legal advocacy to navigate the procedural hurdles and counter insurer tactics.
Time limits apply, so prompt action is crucial. If your family is facing the devastating consequences of a preventable brain injury, we encourage you to seek a free consultation to have your questions answered, understand your options, and move your case forward with confidence to secure the resources necessary for recovery and long-term stability.