At the Law Offices of Anidjar and Levine, we help Floridians harmed by hospital-acquired infections build strong claims through evidence-driven investigations, preserved records, and qualified expert reviews.
We analyze infection-control data, compare hospital practices against CDC and Florida standards, and identify every responsible party.
Our team manages insurer and hospital communications, quantifies medical costs, lost income, and future care, and complies with Florida’s presuit and statute-of-limitations requirements.
We prepare for settlement or trial with disciplined case management and transparent fees.
Continue to see how we protect your rights and maximize recovery, and learn more here: Medical Malpractice Injury Lawyer.
Key Takeaways
- We investigate HAI cases statewide in Florida, coordinating records, expert reviews, and evidence preservation to prove negligence, causation, and damages.
- Our team audits sterilization logs, equipment tracking, cultures, and policies against CDC and Florida standards to identify protocol breaches and sources of infection.
- We handle all insurer and hospital communications, build leverage with evidence-driven demands, and litigate decisively when a settlement is inadequate.
- We pursue full compensation: medical costs, lost income, future care, and non-economic harms, supported by infectious disease and nursing expert testimony.
- Transparent fees, disciplined case selection, regular client updates, and clear timelines for presuit, mediation, or trial under Florida law.
How We Can Help With Your Florida Hospital-acquired Infection Injury Claim
While every case is unique, we appreciate how to move quickly and decisively to protect your rights after a hospital-acquired infection.
Dig deeper into this subject: Strategic Framework for Litigating Hospital-Acquired Infection Claims in Florida: An Analysis of the Anidjar & Levine Methodolog
We begin by listening carefully, documenting your medical timeline, and identifying protocol breakdowns. Our team coordinates records collection, consults with qualified experts, and preserves evidence to support causation and damages.
Throughout, we practice disciplined patient advocacy, ensuring your voice remains central, and your goals guide our strategy.
We manage communications with insurers and hospitals, shielding you from pressure while building leverage through meticulous case development. We calculate full losses, including medical care, lost income, and long-term needs, and we present precise demands supported by evidence.
In settlement negotiation, we prepare as if for trial, which strengthens your position and promotes fair resolution. If negotiation fails, we litigate with precision, filing timely actions and advancing your claim through motions and hearings. Our focus is accountability, safety, and meaningful outcomes.
Understanding Florida Hospital-acquired Infection Injury Cases
Having outlined how we build and advance your claim, we now explain what makes Florida hospital-acquired infection cases distinct and how the law views them. These matters turn on whether a facility met the professional standard of care, documented prudent protocols, and responded promptly to warning signs.
We examine whether infection surveillance programs functioned as required, whether staff followed isolation and sterilization practices, and whether leadership enforced compliance.
Florida’s statutes and regulations shape what’s reasonable for hospitals, physicians, and nurses. We connect those obligations to your medical records, culture results, and timelines to show causation and damages.
Patient education also plays a role, because providers must communicate clear precautions, discharge instructions, and follow-up plans that reduce risk.
To establish liability, we rely on qualified experts, audit trails, and policy manuals, then compare them to state and federal guidance. We also assess charting gaps, delay patterns, and adverse event reports that reveal preventable lapses.

Common Causes of Florida Hospital-acquired Infection Injuries
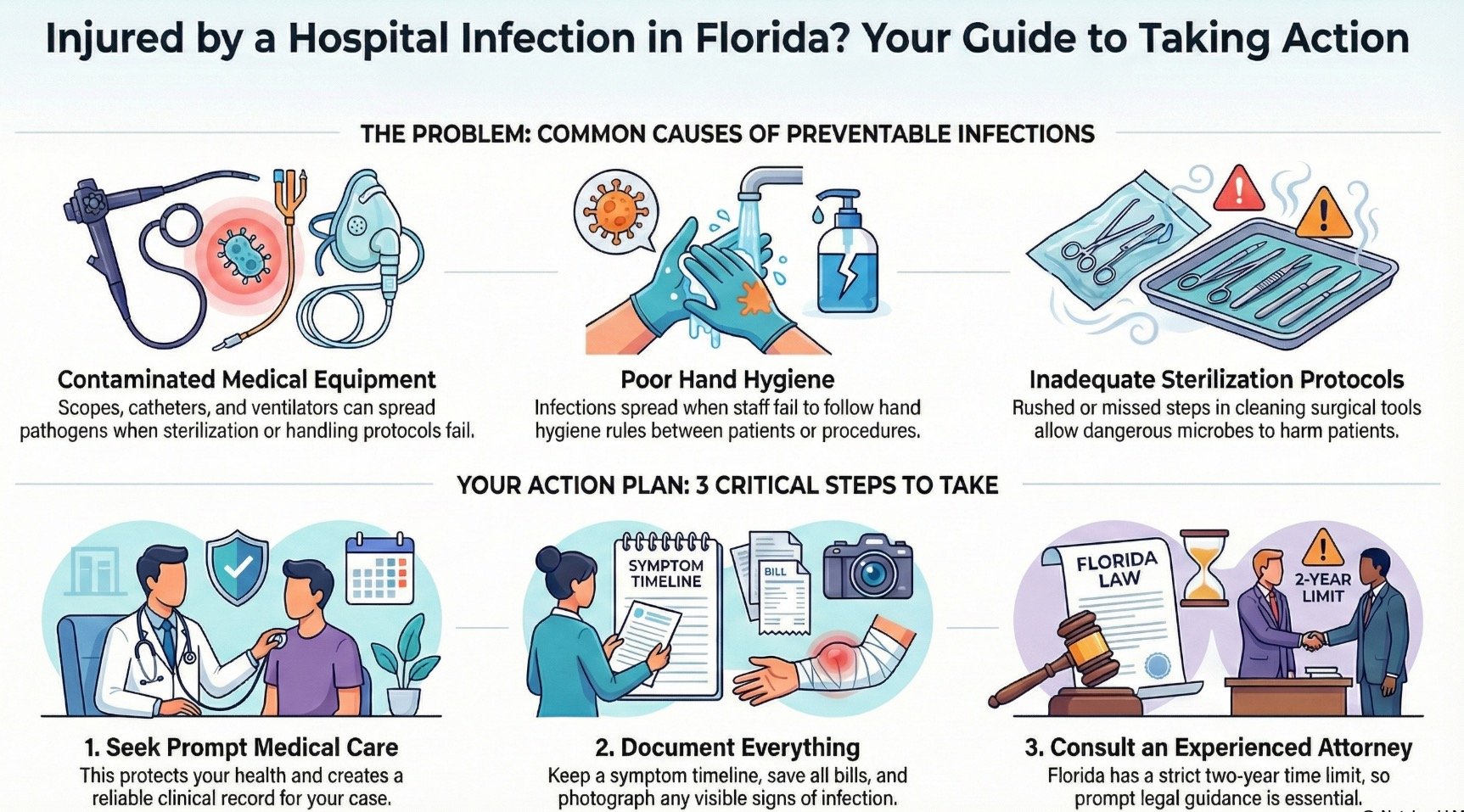
We now examine the most frequent causes of Florida hospital-acquired infection injuries, focusing on contaminated medical equipment and poor hand hygiene that allow pathogens to spread.
We also assess how improper antibiotic use fosters the emergence of resistant organisms, increasing the risk and severity of infections.
Finally, we review inadequate sterilization protocols, identifying where breakdowns in cleaning, disinfection, and oversight lead to preventable harm.
Contaminated Medical Equipment
Breakdowns in equipment sterilization and handling can open the door to dangerous pathogens, turning routine care into a serious infection risk. When devices aren’t properly cleaned, maintained, or tracked, bacteria and fungi can persist, move between patients, and escalate into severe infections.
We evaluate sterilization logs, maintenance records, and chain-of-custody procedures to identify where protocols failed.
Contaminated scopes, catheters, ventilators, and reusable instruments often result from lax oversight, faulty reprocessing, or missed equipment recalls.
We also scrutinize supply contamination, including compromised packaging and storage conditions that allow microbial growth. Hospitals must implement validated cleaning cycles, verify biological indicators, and promptly remove defective devices from service.
If lapses led to your infection, we’re prepared to secure accountability, demand corrective actions, and pursue compensation for medical costs, lost wages, and future care.
Poor Hand Hygiene
Too often, preventable infections trace back to lapses in basic hand hygiene, allowing pathogens to move from surfaces, equipment, and healthcare workers’ skin to vulnerable patients. When hospitals fail to enforce consistent protocols, risk escalates for those already vulnerable.
We expect staff to perform hand hygiene at every key moment of care, yet gaps occur during hurried shifts, room entries, or device handling.
Effective prevention requires clear policies, reliable supplies, and accountability. Facilities should adopt evidence-based soap formulations and alcohol-based rubs that balance antimicrobial efficacy with skin tolerance, supporting routine use.
Strong compliance monitoring, including direct observation and electronic auditing, identifies patterns and enables timely correction. Targeted behavioral interventions, reinforced by leadership and peer modeling, drive sustained adherence and protect patients from avoidable harm.
Improper Antibiotic Use
Frequently overlooked yet profoundly consequential, improper antibiotic use fuels many hospital-acquired infections by selecting for drug‑resistant organisms and disrupting normal microbial defenses.
When clinicians prescribe broad-spectrum drugs without clear indications or continue therapy longer than necessary, patients face heightened risks of C. difficile and multidrug-resistant pathogens.
We evaluate records for guideline deviations, missed cultures, and failures to de-escalate therapy, because these lapses often trace directly to preventable harm.
As your advocates, we emphasize antibiotic stewardship and resistance prevention as core duties owed to every patient. Hospitals must implement protocols that verify diagnosis, narrow coverage promptly, and monitor dosing and duration. When systems ignore these safeguards, the standard of care falters. We build cases with expert review, causation analysis, and damages documentation to pursue accountability and safer practices.
Inadequate Sterilization Protocols
Lapses in sterilization allow dangerous pathogens to move from one patient to the next, turning routine care into a source of serious infection. When a surgical tool isn’t properly cleaned, disinfected, and sterilized, microbes can persist, enter the body, and cause preventable harm.
We expect hospitals to follow validated protocols, yet breakdowns occur when staff skip steps, documentation is incomplete, or cycles are rushed.
We look for evidence of systemic failures, including missed sterilization audits, inadequate autoclave maintenance, and weak infection surveillance. Poor instrument tracking, improper packaging, and incorrect cycle parameters often reveal a pattern of neglect.
By examining training records, maintenance logs, and quality reports, we identify where standards were ignored. When preventable infections result, we pursue accountability and safer practices for every patient.
Legal Rights of Florida Hospital-acquired Infection Injury Victims
Although every case turns on its facts, Florida patients harmed by hospital-acquired infections have clear legal rights grounded in medical negligence, premises liability, and, at times, product liability.
We have the right to expect reasonable infection control, accurate documentation, and transparent communication.
When those duties are breached, we may seek compensation for medical costs, lost income, and pain and suffering.
Informed Patient consent matters, and failures to disclose material risks or alternatives can support a claim.
We also safeguard your interests during Insurance disputes, ensuring benefits are honored and bad-faith tactics are challenged.
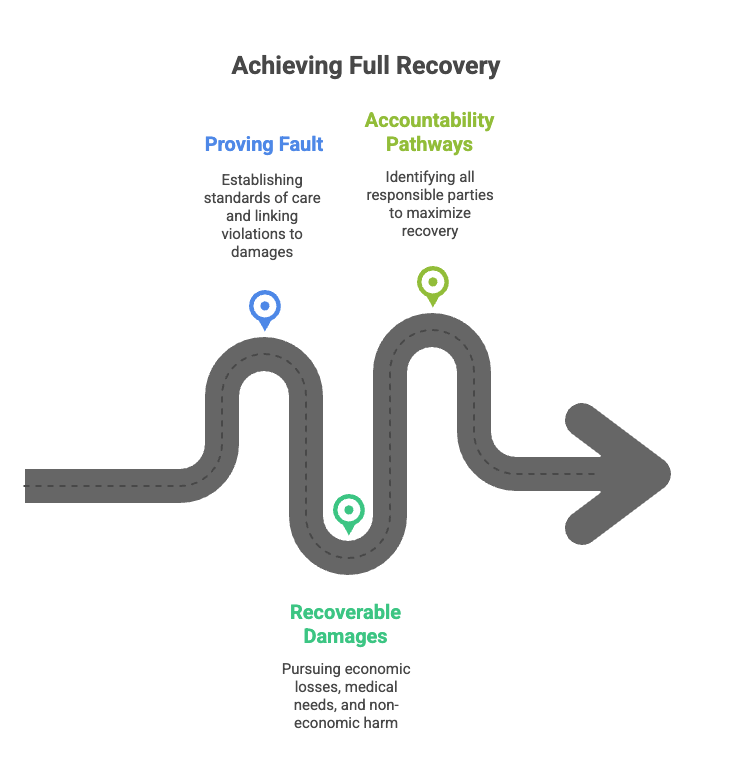
- Proving fault: We establish standards of care, show how they were violated, and link those failures to the infection and damages.
- Recoverable damages: We pursue economic losses, future medical needs, and non-economic harm, with expert support to quantify each category.
- Accountability pathways: We evaluate hospitals, contractors, and product manufacturers, identifying every responsible party to maximize lawful recovery.
Steps to Take After a Florida Hospital-acquired Infection Injury
When a hospital-acquired infection is suspected, we should urge you to seek prompt medical care to stabilize your condition and create a reliable clinical record.
We then recommend that you document symptoms, test results, medications, and all related communications, preserving bills, discharge summaries, and timelines.
Finally, we encourage you to consult an experienced attorney without delay, so we can protect evidence, evaluate liability, and guide next steps under Florida law.
Seek Prompt Medical Care
From the outset, seek prompt medical care at the first sign of a hospital-acquired infection, such as fever, unexpected pain, redness or swelling around surgical sites, unusual drainage, or sudden fatigue. Early action protects health, curbs complications, and supports safer outcomes for you and those who depend on you.
We encourage immediate evaluation by a qualified clinician, because early diagnosis allows timely antibiotics, wound care, or isolation measures that can prevent escalation.
If you can’t reach your provider quickly, visit urgent care or an emergency department, and disclose recent procedures, devices, and medications. Ask for targeted testing and clear return precautions.
Use telemedicine follow up to maintain close oversight, confirm treatment effectiveness, and adjust care plans. Prompt, coordinated attention strengthens recovery and reduces avoidable harm.
Document Symptoms and Treatment
Consistently document every symptom and treatment step to create a clear medical and legal record.
We begin by maintaining a daily symptom timeline, noting onset, intensity, duration, triggers, and relief. We include fever readings, pain scores, wound changes, and any new limitations.
We meticulously preserve treatment records , including prescriptions, lab results, culture reports, imaging, discharge summaries, and instructions. We save appointment dates, provider names, and communications, including patient portal messages and phone logs.
We photograph visible signs—redness, swelling, or drainage—using date stamps, and we align these images with our symptom timeline. We track work absences and caregiving impacts, because functional losses corroborate clinical data. We keep receipts for medications, supplies, and travel.
This disciplined approach strengthens causation, demonstrates diligence, and supports fair resolution.
Consult an Experienced Attorney
Although medical records and timelines help establish what happened, we protect our rights by consulting a Florida attorney who regularly handles hospital-acquired infection cases. We should reach out promptly, because early legal guidance helps preserve evidence, identify liable parties, and avoid missed deadlines.
An experienced firm will perform a structured case intake, review our documentation, and advise on next steps with clarity and candor.
During client interviews, we’ll discuss our observations of their symptoms, procedures, and infection-control lapses. We should ask about the attorney’s experience, investigation methods, and communication practices. The lawyer may secure expert reviews, request additional records, and send preservation letters.
If representation is appropriate, we’ll receive a written agreement outlining fees and responsibilities. Swift counsel strengthens our claim and protects our recovery.
How a Florida Hospital-acquired Infection Injury Lawyer Can Help You
Secure clarity and control by engaging counsel who understands how hospital-acquired infection cases are built and won. We coordinate investigations, preserve records, and work with medical experts to identify breaches in protocols and causation. Our approach centers on patient advocacy, ensuring your voice guides strategy and settlement decisions. We pursue accountability while respecting the caregiving mission, balancing firmness with professionalism.
We gather infection-control data, analyze hospital policies, and compare them with state and federal standards. We then quantify losses, from medical expenses to lost income, and negotiate with insurers using evidence-driven demands. When necessary, we litigate decisively, presenting clear narratives that align with community health values and responsible care.
- Evidence mapping and expert alignment to prove negligence, causation, and damages.
- Strategic negotiations that leverage regulations, sentinel event data, and compliance gaps.
- Courtroom advocacy that seeks compensation and supports policy reform to prevent future harm.
We stand beside you, focused on results and systemic improvement.
Long-Term Effects of Florida Hospital-Acquired Infection Injuries
When hospital-acquired infections linger, we face chronic health complications that can impair organ function, mobility, and overall resilience.
We also recognize the psychological and emotional impact, including anxiety, depression, and trauma symptoms that can persist long after discharge.
Finally, we must account for the financial and lifestyle burdens, as ongoing treatment, reduced earning capacity, and daily limitations reshape a patient’s future.
Chronic Health Complications
Often overlooked in the immediate aftermath of a hospital-acquired infection, the long-term consequences can persist for months or years and reshape a patient’s health trajectory.
We frequently see infection sequelae, including organ dysfunction, impaired wound healing, antibiotic-resistant recurrences, and mobility limitations. These conditions demand coordinated, chronic management that balances medications, rehabilitation, and vigilant follow-up.
We help you document complications, track triggers, and align care plans with experts who understand post-infection physiology.
For some, cardiac strain, renal impairment, or respiratory compromise becomes a persistent risk. Others face diabetic decompensation, vascular injury, or joint damage following septic arthritis. We work to secure resources for durable medical equipment, home health, and transportation, ensuring continuity of care.
By proving causation and future needs, we position claims to cover lifelong treatment and preserve dignity.
Psychological and Emotional Impact
Though the infection may resolve, its psychological footprint can linger, shaping daily life in ways that are no less debilitating than physical symptoms. We often see anxiety, sleep disruption, and intrusive memories tied to hospitalization, mainly when isolation or painful procedures occurred.
Trust in medical settings may fracture, and that distrust can complicate follow-up care. We address these harms directly, recognizing that mental health injuries require validation, structured support, and careful documentation.
We work with clinicians to identify PTSD symptoms, depressive episodes, and health-related phobias, building a clear record that reflects lived experience. Through a trauma recovery lens, we encourage consistent therapy, evidence-based treatments, and supportive networks.
Financial and Lifestyle Burdens
Emotional injuries shape choices, and those choices carry price tags that accumulate long after discharge.
When infections derail recovery, we confront mounting medical bills, transportation costs, and home-care expenses that strain family budgets.
Lost wages compound the pressure, especially when extended leave or job separation follows prolonged treatment.
Caregivers often reduce hours or exit the workforce, shifting income and benefits downward.
We also face necessary Lifestyle adjustments.
Mobility aids, wound supplies, and home modifications become recurring costs, not one-time fixes.
Physical therapy and follow-up appointments demand time, coordination, and reliable support.
Children, elders, and community commitments may be reshuffled to protect health and prevent reinjury.
Our role is to document these burdens precisely, connect you with resources, and pursue compensation that reflects long-term realities.
Proving Liability in Florida Hospital-acquired Infection Medical Malpractice Injury Cases
Establishing liability in a Florida hospital-acquired infection case demands a methodical showing that the facility breached the applicable standard of care and that this breach caused the infection and resulting damages.
We begin by identifying the precise infection source through infection tracing, reviewing procedure logs, isolation protocols, and hand hygiene compliance. We corroborate these findings with microbiology testing, including cultures, antibiograms, and genetic typing, to link the pathogen to a contaminated device, unit, or staff practice.
We then measure conduct against authoritative standards, such as CDC and professional guidelines, to show where practices fell short. Expert testimony from the infectious disease and nursing standards authority connects policy failures to the infection event. We also examine staffing levels, credentialing, and equipment maintenance to expose systemic negligence.
Finally, we establish causation with a clear timeline, demonstrating the absence of the pathogen at admission and its emergence following negligent exposure, supported by medical records and expert analysis.
Compensation for Florida Hospital-acquired Infection Damages
Having shown how negligence caused the infection and resulting harm, we next quantify what full and fair compensation should cover under Florida law.
We begin with economic losses: past and future medical expenses, hospitalization, surgeries, rehabilitation, home health aids, and necessary medications. We document lost wages, diminished earning capacity, and attendant care.
We also pursue non-economic damages for pain and suffering, loss of enjoyment of life, scarring, and disability, translating daily hardships into credible, evidence-based valuations.
Our patient advocacy approach demands a careful accounting of future needs, including infectious disease follow-up, prosthetics, and mental health care for trauma and anxiety. We retain experts to connect each category of loss to the medical negligence, using records, bills, life-care plans, and vocational assessments.
We also assess household services, transportation, and caregiver burdens.
Where egregious conduct appears, we evaluate punitive exposure to deter similar harm. Throughout, we center your recovery, ensuring compensation reflects the full impact on your life and family.
The Statute of Limitations for Florida Hospital-acquired Infection Injury Cases
Although each case turns on specific facts, Florida imposes strict deadlines that govern when we can file a hospital-acquired infection malpractice claim. Generally, the statute of limitations is two years from the time we knew or should have known that negligence caused the infection, a standard guided by the discovery rule.
There’s also a four-year statute of repose that can bar claims regardless of discovery, emphasizing the need for early action.
Before filing, Florida requires presuit investigation steps, which consume time and must be accounted for when calculating deadlines. Certain statute exceptions may extend or toll the period, including cases involving fraud, concealment, or a foreign object, and situations where the injured person is a minor or legally incapacitated.
Wrongful death claims follow a distinct two-year limit.
We work methodically to document timelines, preserve evidence, and comply with every statutory requirement. We’d like to let you know that prompt consultation allows us to evaluate deadlines accurately and protect your right to pursue relief.
Why You Need an Experienced Florida Hospital-acquired Infection Injury Lawyer
Time limits and presuit demands mean the right lawyer isn’t just helpful—it’s decisive. Hospital-acquired infection cases move quickly, and we must preserve evidence, consult experts, and satisfy statutory requirements without delay. An experienced Florida lawyer understands the medical records, infection control standards, and causation hurdles that determine success.
Deadlines are unforgiving—experienced Florida counsel secures evidence, experts, and compliance to win hospital-acquired infection cases.
We bring disciplined case selection, ensuring your resources and energy are focused on claims with substantial liability and provable damages. That discernment prevents wasted time and positions your case for early leverage.
Skilled counsel coordinates medical reviews, identifies systemic breakdowns, and quantifies lifelong costs for care, wage loss, and support.
Clear client communication anchors every step. We explain risks, share timelines, and prepare you for pre-suit investigations, mediation, and litigation. Insurers respond to thorough documentation and credible expert testimony, which we develop methodically.
With experience, we anticipate defenses, negotiate from strength, and, when necessary, try the case to protect your recovery and your dignity.
How to Choose the Right Florida Hospital-acquired Infection Injury Lawyer for Your Case
When stakes are high and facts are technical, choosing the right Florida hospital-acquired infection lawyer requires deliberate, criteria-driven evaluation. We start by verifying specific experience with healthcare-associated infections, medical standards, and hospital policies.
We then assess litigation results, settlement outcomes, and trial readiness, because insurers respond to proven advocacy. During client interviews, we evaluate clarity, responsiveness, and compassion to ensure your story is heard and documented with precision.
We examine investigative resources, including access to infectious disease experts, nurse consultants, and data analysts. We confirm the firm’s capacity to preserve evidence, manage intricate discovery, and challenge defense experts.
Fee structures must be transparent, with written terms covering costs, liens, and potential appeals. We expect candid risk assessments, realistic timelines, and proactive communication plans.
Finally, we look for alignment with service-oriented values. The right lawyer safeguards your health, finances, and dignity while advancing systemic accountability to protect other patients.
About the Law Offices of Anidjar and Levine
Built on disciplined advocacy and client-centered service, the Law Offices of Anidjar and Levine is a Florida firm focused on detailed injury litigation, including hospital-acquired infection cases.
We bring a meticulous approach to evidence, timelines, and expert testimony, ensuring your claim is positioned for maximum recovery.
Our team coordinates medical reviews, preserves essential records, and negotiates strategically, while preparing every matter as if it will proceed to trial.
We measure our performance by results and by how we serve.
Client testimonials reflect consistent communication, clear guidance, and steadfast follow-through. We return calls, provide case updates, and make complicated decisions understandable, so you can focus on healing while we advance your case.
Our commitment extends beyond the courtroom. Through community outreach, we support patient safety initiatives, professional education, and local health programs, reinforcing standards that prevent avoidable harm.
When you hire us, you gain disciplined advocates who protect your rights, honor your voice, and pursue accountable outcomes.

Frequently Asked Questions
Will Filing a Claim Affect My Ongoing Medical Treatment at the Hospital?
No, filing a claim shouldn’t affect your ongoing medical treatment. We prioritize your patient rights and expect the hospital to uphold professional standards, ensuring treatment continuity without retaliation.
Your care team must focus on your health, maintain confidentiality, and avoid conflicts that could compromise outcomes. If you notice delays, dismissive behavior, or changes in access, we’ll document the concerns, request a care reassignment if needed, and escalate through patient advocacy, risk management, or external regulators to ensure uninterrupted care.
Can I Switch Doctors During My Infection Recovery Without Hurting My Case?
Yes, you can change doctors during the recovery from an infection, and doing so need not hurt your case. We’ll protect the record by ensuring continuity concerns are addressed: obtain complete medical records, maintain consistent treatment plans, and document reasons for the switch, such as specialized knowledge or communication needs.
We’ll notify insurers promptly, coordinate referrals, and align providers on diagnosis and prognosis. When handled carefully, the change can enhance care quality while preserving credibility and evidentiary integrity.
How Do I Preserve Contaminated Device or Dressing Evidence Safely at Home?
We preserve contaminated items by sealing them in clean, labeled containers, avoiding cleaning or alteration.
We photograph the item and site thoroughly, ensuring clear, timestamped documentation.
We handle items with gloves, place items in separate bags, and record each transfer to maintain a strict chain of custody.
We store them in a cool, dry place, away from sunlight.
We also want to note the dates, locations, and witnesses, and we’d like some guidance from healthcare and legal professionals.
Are Interpreter Services Available for Non-English-Speaking Clients During the Case?
Yes, we provide interpreter services for non‑English‑speaking clients throughout the case. We coordinate professional interpreters for meetings, depositions, medical consultations, and court proceedings, ensuring reliable language access.
We train our team in cultural competency to respect the nuances that affect testimony, consent, and decision‑making. We confirm interpreter credentials, maintain confidentiality, and schedule services proactively.
We also translate essential documents, verify understanding at each stage, and remain available to address urgent communication needs.
Can Telehealth Visits Substitute for In-Person Follow-Ups for Documentation?
Yes, telehealth visits can supplement, but rarely substitute, in-person follow-ups for documentation. We must account for telehealth limitations, including constrained physical exams, image quality, and identity verification.
For documentation best practices, we recommend detailed visit notes, time-stamped photos, secure messaging records, and consistent symptom tracking. When objective findings are required, we prioritize in-person evaluations, timely diagnostics, and clinician-signed reports.
Collectively, we balance convenience with evidentiary reliability to ensure complete, credible records.
————————
We’re ready to protect your rights and pursue the compensation you deserve after a hospital-acquired infection.
Our team investigates the facts, secures medical and expert evidence, and builds a precise, persuasive claim.
We’ll manage insurers, deadlines, and litigation, allowing you to focus on recovery.
Time limits apply, so prompt action matters. Contact the Law Offices of Anidjar & Levine for a free consultation, and let us put our experience, resources, and resolve to work for you.
Learn more here: Medical Malpractice Injury Lawyer