Introduction: The Diagnostic Blind Spot
At the intersection of modern medical practice and Florida law lies a significant diagnostic blind spot: the misread radiology scan. While imaging technology has advanced, the interpretive and systemic failures that lead to these errors remain a persistent source of preventable patient harm and complex litigation.
Read More: Florida Misread Radiology Scan Injury Lawyer
An error in interpretation—a missed fracture, an overlooked lesion, or a misclassified finding—can initiate a cascade of devastating consequences, derailing effective treatment, allowing diseases to progress unchecked, and imposing profound physical, emotional, and financial burdens.
The purpose of this case study is to dissect the lifecycle of a typical misread radiology scan claim in Florida, from the initial diagnostic error to the legal resolution.
This analysis will explore the key areas that define such a case: the legal standard of care that radiologists must meet, the common systemic and human causes of diagnostic failure, the long-term impact these errors have on patients, and the strategic legal steps required to establish liability and secure just compensation.
——————————————————————————–
1. The Foundational Error: Defining a Breach of Care
The basis of any medical malpractice claim, including one arising from a misread scan, is a “breach of the standard of care.” Precisely defining this breach is the essential first step in building a viable case. It is not enough to show that an error occurred; one must demonstrate that the radiologist or institution failed to provide a level of care that a reasonably prudent peer would have offered under similar circumstances.
The legal analysis of a misread scan claim in Florida is built upon two core components:
- Breach of Standard of Care: This concept is evaluated by asking what a “reasonably prudent radiologist” would have done with the same imaging, clinical information, available tools, and training. The claim must establish that the interpretation fell below this accepted professional benchmark, resulting in a missed or incorrect finding that a competent peer would have identified.
- Causation of Preventable Injury: Proving a breach is only half the battle. It is equally critical to prove that the misreading was a direct cause of a worsened outcome. This involves demonstrating how the error led to tangible harm, such as lost treatment opportunities, the need for more invasive or costly procedures, or the progression of a disease to a more advanced stage.
Beyond an individual practitioner’s error, liability often extends to the institution. Systemic negligence and technological failures create an environment where diagnostic biases are more likely to lead to a breach of care. For example, an institution’s failure to implement a robust peer-review process or mandate double reads on high-risk studies constitutes a systemic failure. Likewise, the failure to responsibly upgrade imaging technology can lead to poor image quality. These institutional gaps directly contribute to conditions where cognitive errors like “anchoring” on an initial impression or “premature closure” of the diagnostic process are more likely to occur and go uncorrected, forming a clear basis for institutional liability.
Having established the legal definition of a breach, the next step is to deconstruct the common operational failures—from poor image quality to systemic communication gaps—that give rise to such a breach in a clinical setting.
——————————————————————————–
2. Deconstructing the Failure: Common Causes of Misread Scans
Diagnostic errors are rarely the result of a single, isolated mistake. More often, they are the predictable outcomes of systemic vulnerabilities, process gaps, or a combination of human and technical factors. Understanding these root causes is crucial for proving liability, as it allows for a precise identification of where the diagnostic process failed and who bears responsibility. The most common causes of misread scans can be traced to four primary areas of failure.
Inadequate Image Quality
It is a dangerous myth that any scan is “good enough” for interpretation. In reality, inadequate image quality is a leading driver of diagnostic errors. When images are compromised by technical issues like motion artifacts that blur critical structures or contrast insufficiency that fails to differentiate tissues, vital pathological findings can be obscured or distorted. Contributing factors often include poor patient positioning, the use of improper scanning protocols, and reliance on outdated or poorly maintained equipment, all of which degrade clarity and undermine the potential for an accurate diagnosis.
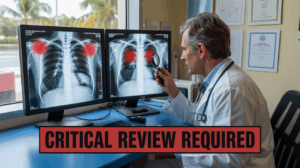
Radiologist Interpretation Errors
Even with high-quality images, the interpretive skill of the radiologist remains paramount. Errors in this phase often arise from cognitive biases such as confirmation bias (seeing what one expects to see) or anchoring (over-relying on an initial piece of information). Rushed workflows and fatigue are also significant contributors, leading to missed findings like small lesions, subtle fractures, or the early signs of a stroke. Systemic safeguards designed to mitigate these human factors include mandatory peer review of a percentage of cases and requiring second reads for high-risk studies. The complementary use of artificial intelligence to flag potentially overlooked findings is an emerging standard. However, over-reliance on AI or its use as a substitute for, rather than an enhancement of, expert human interpretation can itself constitute a breach of care, creating new avenues for liability.
Communication Breakdowns
A correct interpretation is of little value if it is not communicated effectively and in a timely manner. Errors frequently occur at the “interfaces” between the radiologist, the ordering provider, and the patient. Gaps arise when urgent results are not escalated properly, often languishing in a passive electronic inbox instead of being communicated via direct contact. Disciplined communication protocols are the antidote to such failures. Key elements include ensuring role clarity among clinicians so that responsibilities for acting on a finding are clear and maintaining well-defined report distribution lists to ensure all necessary members of the care team are informed. A failure to standardize these critical communication pathways is a frequent source of preventable harm.
Delayed Follow-Up Testing
The diagnostic process does not always end with a single report; often, an initial finding requires prompt follow-up imaging to confirm a diagnosis or monitor a condition. A failure to schedule, track, or perform this necessary follow-up allows diseases to progress unchecked, erasing the benefits of an early potential discovery. A robust follow-up system includes defined responsibilities for who orders and tracks subsequent tests, automated patient reminders, and a system of closed-loop result acknowledgment to confirm that the care team is aware of the need for further action. A deviation from such safeguards, resulting in a harmful delay, can constitute negligence.
Understanding these points of failure is essential not only for establishing legal accountability but also for appreciating the severe, long-term consequences that unfold for the patient.
——————————————————————————–
3. The Human Cost: Long-Term Consequences of Diagnostic Delay
The harm caused by a misread radiology scan extends far beyond the immediate medical issue that was missed. The true impact unfolds over time, creating a ripple effect that touches every aspect of a patient’s life, including their physical health, emotional well-being, and long-term financial stability. A single diagnostic error can trigger a cascade of negative consequences that fundamentally alters a person’s future.
Complications from Delayed Diagnosis
A delayed diagnosis can set off a chain reaction of clinical complications. For example, tumors may upstage from a treatable early stage to a more advanced and dangerous one. Infections can spread, becoming systemic and life-threatening. Fractures may heal improperly, leading to chronic instability and pain. As the condition worsens, treatment options that were once minimally invasive and highly effective may become riskier, costlier, or no longer viable at all. This forces patients to undergo more aggressive and debilitating therapies that could have been avoided with a timely and accurate diagnosis.
Progression to Chronic Pain
When injuries are not identified and treated promptly, acute pain can evolve into a debilitating chronic condition. Untreated structural damage, persistent inflammation, and ongoing nerve irritation can create a vicious cycle of pain and reduced mobility. This can lead to progressive neuropathy, muscle guarding, and joint stiffness, fundamentally impairing a person’s ability to perform daily activities, work, or engage in meaningful hobbies. What may have started as a manageable injury becomes a life-altering source of constant suffering.
The Psychological and Financial Toll
The psychological toll of a misread scan constitutes a significant component of non-economic damages. Patients grapple with documented anxiety, a quantifiable loss of confidence in the healthcare system, and profound family strain, all of which must be translated into the valuation of the claim. The financial toll can be equally devastating. The costs of unexpected and more intensive treatments accumulate quickly, compounded by lost income from being unable to work. Projecting the costs of future care, rehabilitation, and necessary assistance adds another layer of financial stress, creating a profound sense of instability for patients and their families.
The sum of these damages—physical, emotional, and financial—forms the basis of the legal process required to pursue compensation and accountability in Florida.
——————————————————————————–
4. The Path to Accountability: Navigating a Florida Malpractice Claim
While a patient’s right to competent medical care is clear, enforcing that right after a misread scan requires navigating a precise and time-sensitive legal framework. The discovery of a diagnostic error necessitates strategic, methodical action to protect both the patient’s health and their legal claim.
Following the discovery of a suspected misread scan, a patient must take several immediate and critical steps:
- Seek Immediate and Correct Medical Care: The absolute first priority is to safeguard one’s health. This involves obtaining an urgent evaluation to stabilize any hidden condition, prevent further harm, and officially document the correct diagnosis, which becomes a crucial piece of evidence.
- Preserve All Imaging and Records: It is vital to secure all related evidence in its original format. This includes requesting complete copies of radiology images (in DICOM format), the associated reports, technician notes, and physician orders. Maintaining a clear chain of custody without altering any original files is essential for evidentiary integrity.
- Consult a Specialized Florida Injury Attorney: Early legal counsel is vital for protecting the claim. Florida has strict procedural rules and deadlines, and an experienced attorney can ensure these are met, evaluate the merits of the case, and guide all subsequent actions.
The Florida Statute of Limitations
Timeliness is critical. Florida law imposes strict deadlines for filing a medical malpractice claim:
- A claimant has two years from the date they knew, or reasonably should have known, about the injury and its potential connection to medical negligence. This is known as the “discovery rule.”
- There is also a four-year absolute deadline from the date the malpractice occurred, known as the “statute of repose,” which can bar a claim even if it was discovered later.
- The law allows for limited tolling (pausing) of these deadlines in specific circumstances, such as cases of fraudulent concealment by the provider or when the patient is a minor.
Proving Liability
Successfully navigating a claim requires building a legally sound case that clearly demonstrates negligence and harm. This process involves several key actions:
- Establishing a clear deviation from the accepted medical standard of care for a radiologist.
- Linking the misread scan to specific, measurable harm through a clear and well-documented medical timeline.
- Securing qualified expert testimony from board-certified specialists whose opinions on the breach and causation are grounded in Florida law.
- Authenticating all radiology data, including the original DICOM files and their associated audit trails, to show what information was available to the radiologist at the time of the interpretation.
- Satisfying Florida’s mandatory pre-suit requirements, which involve providing detailed notice to the healthcare provider before a lawsuit can be filed.
Successfully navigating these complex steps requires a deep understanding of both medicine and Florida law, which is why the guidance of experienced legal counsel is often indispensable.
——————————————————————————–
5. Securing Justice: Compensation and the Role of Expert Counsel
The ultimate goal of a medical malpractice claim is to secure full and fair compensation that addresses the entire scope of a patient’s losses. Achieving this outcome requires specialized legal advocacy capable of translating the profound harm caused by a misread scan into a comprehensive and defensible valuation. In Florida, victims are entitled to seek compensation for a range of damages.
The types of compensation available can be categorized as follows:
| Category of Damages | Description and Examples |
| Economic Damages | These are tangible, verifiable financial losses. Examples include all past and future medical expenses, future treatment costs, the costs of rehabilitation and assistive devices, lost wages from time away from work, and diminished earning capacity if the injury prevents a return to a previous career. |
| Non-Economic Damages | These are intangible losses related to the impact on a person’s quality of life. This category includes compensation for physical pain and suffering, loss of enjoyment of life, and the severe emotional burden and anxiety that accompany a delayed diagnosis and its consequences. |
| Punitive Damages | While less common, these damages are not intended to compensate the victim but rather to punish the defendant for egregious conduct. They may be pursued “when warranted” under the specific requirements of Florida law. |
Securing this compensation requires the skill of an experienced misread radiology scan injury lawyer, who performs several critical functions to build and advance the case:
- Case Evaluation and Strategy: The process begins with a meticulous analysis of medical records, imaging studies, and applicable standards of care to develop a targeted liability plan designed to prove negligence and causation.
- Expert Engagement: A crucial role is retaining highly qualified, board-certified medical experts. These specialists are essential for substantiating the breach of care, linking the error directly to the patient’s harm, and quantifying the full extent of the damages.
- Evidence Development: Counsel is responsible for obtaining all necessary evidence beyond the patient’s own records. This includes demanding hospital policies on reporting and peer review, securing digital audit trails of the imaging files, and conducting depositions of all involved parties to clarify fault.
- Negotiation and Resolution: By preparing every case as if it will go to trial, a lawyer builds a litigation-ready position of strength. This leverage is used to negotiate a fair settlement that provides just results for the client, avoiding the need for a trial whenever possible.
This methodical and expert-driven approach is designed to ensure that the final resolution fully accounts for the harm done, providing the resources necessary for recovery and future stability.
——————————————————————————–
6. Strategic Considerations: Answering Key Questions in a Radiology Malpractice Claim
Navigating a radiology malpractice claim involves more than just understanding the core legal principles; it also requires addressing complex strategic questions that frequently arise for patients and their families. The answers to these questions can significantly impact both medical recovery and the legal outcome.
Can I change radiologists after a misread without harming my case? Yes, you can and should change providers to ensure you receive proper care. This action will not harm your case, provided it is handled carefully. It is important to formally notify the providers in writing, request complete copies of all imaging and reports to ensure continuity of care, and preserve all original records. This process protects your medical interests while safeguarding the evidentiary integrity of your legal claim.
Will my health insurer demand reimbursement from any settlement? Yes, it is very likely. Many health insurance policies, especially ERISA plans, contain subrogation clauses giving the insurer a right to be reimbursed for medical expenses they paid related to the injury from any settlement or verdict. An experienced attorney can verify the insurer’s legal rights, negotiate reductions based on legal principles like the common-fund and made-whole doctrines where applicable, and challenge excessive claims to maximize your net recovery.
Are second-opinion radiology reviews confidential during a lawsuit? They can be, if structured correctly. When a second-opinion review is retained by your attorney as part of the legal investigation, it is typically protected by the attorney-client relationship and the work-product doctrine. This allows your legal team to develop its strategy in confidence. These protections remain in place unless you and your counsel decide to disclose the expert’s findings as part of the case.
Can I sue a tele-radiology company based outside of Florida? Yes, it is often possible to sue an out-of-state tele-radiology company if they provided services that caused harm in Florida. The legal question centers on jurisdiction—whether the company has sufficient connections to Florida to be brought into court here. Courts typically look at where the medical services were directed and where the harm occurred. This process involves complex legal arguments and procedural rules for serving an out-of-state defendant.
How do misread scans affect life insurance or disability claim approvals? A misread scan can create inconsistencies in your medical record that insurers may use to deny, delay, or reduce benefits on life or disability policies. To counter this, it is essential to correct the record with the accurate diagnosis, supported by physician affidavits and a clear timeline. Proactively addressing these discrepancies with meticulous documentation is key to restoring eligibility and securing the benefits to which you are entitled.
Proactive management of these strategic issues is a hallmark of effective legal representation and is crucial for achieving a successful outcome.
——————————————————————————–
Conclusion: From Error to Accountability
This case study has illuminated the complex journey from a diagnostic blind spot to legal accountability. A misread radiology scan is not a minor oversight; it is a serious event with the potential to inflict profound and lasting harm on a patient’s health, financial stability, and overall quality of life. The failure can stem from poor image quality, human error, communication breakdowns, or systemic neglect within a healthcare institution.
The central message is clear: while the consequences of a diagnostic error are severe, Florida law provides a defined pathway to hold negligent parties accountable. This path, however, is governed by strict deadlines and requires a meticulous, evidence-based approach to prove that a breach of the standard of care directly caused preventable injury.
For victims of a misread scan, prompt, informed, and expert-guided action is essential to protect their rights, support their recovery, and achieve a just resolution.