If your newborn suffered severe hyperbilirubinemia, the Law Offices of Anidjar and Levine can provide a lawyer who understands neonatal standards, bilirubin thresholds, and how missed monitoring can lead to kernicterus.
We’ll scrutinize charts, bilirubin trends, and treatment timing, preserve crucial evidence, and align expert opinions to establish fault and damages.
With tight deadlines and intricate causation issues, early action matters.
Learn how to protect your child’s future care, verify negligence, and position your claim for maximum compensation.
Speak with a Birth Injury Lawyer today.
Key Takeaways
- Experienced neonatal malpractice attorneys evaluate records, experts, and timelines to prove duty, breach, causation, and damages in hyperbilirubinemia injury cases.
- Prompt consultation preserves evidence, meets deadlines, and coordinates communication with hospitals and insurers while you focus on your child’s care.
- Lawyers compare care to neonatal guidelines on bilirubin monitoring, phototherapy, IVIG, and exchange transfusion to identify preventable failures.
- They gather bilirubin levels, phototherapy logs, discharge instructions, and witness testimony, translating deviations into clear causation opinions.
- Firms often work on contingency, negotiate with insurers, and litigate to secure funds for therapies, life‑care planning, and long‑term needs.
How We Can Help With Your Severe Hyperbilirubinemia Injury Claim
From the outset, we step in to evaluate your case, protect your rights, and build a strategy tailored to the facts of your child’s severe hyperbilirubinemia injury.
You’ll receive clear guidance on immediate next steps, timelines, and decision points, so you can focus on care while we manage the claim.
Clear next steps, timelines, and decisions—so you can focus on care while we manage your claim.
We collect and organize medical documentation, identify pivotal records, and consult qualified experts to substantiate causation and damages.
We coordinate communication with insurers and hospitals, preserving evidence and preventing misstatements that could harm your claim.
Our team assesses liability, calculates full economic and non-economic losses, and crafts a precise demand backed by facts and expert analysis.
When appropriate, we lead settlement negotiations with a disciplined, data-driven approach, pressing for results that reflect the true scope of harm.
If negotiations stall, we prepare for litigation, file timely pleadings, and advocate with resolve, ensuring your voice is heard and your child’s needs remain at the forefront.
Understanding Severe Hyperbilirubinemia Injury Cases
Although every family’s experience is unique, severe hyperbilirubinemia cases share core medical and legal elements you must understand early.
You’ll evaluate how bilirubin metabolism should be monitored from birth, what thresholds trigger intervention, and whether providers followed established protocols.
Accurate documentation of assessments, lab values, and timely escalation is central to liability analysis, because missed signs can allow bilirubin to cross the blood-brain barrier.
You must also examine whether kernicterus prevention steps were applied, including early risk stratification, lactation support, phototherapy, and prompt exchange transfusion when indicated.
Your case hinges on connecting deviations from standards to the injuries documented on neuroimaging, developmental evaluations, and long-term care plans.
Preserve medical records, discharge instructions, and communications, as these materials frame causation and damages.
Finally, you’ll consider future needs such as therapy, assistive technology, and caregiver support, translating them into a life-care plan.
This structured approach safeguards accountability and secures vital resources.
Common Causes of Severe Hyperbilirubinemia Injuries
You should understand that severe hyperbilirubinemia often stems from identifiable medical conditions, including neonatal hemolytic disease and triggers of G6PD deficiency that accelerate red blood cell breakdown.
You may also encounter breastfeeding-associated jaundice when inadequate intake or dehydration increases bilirubin levels, requiring timely monitoring and intervention.
In older infants and children, biliary obstruction can impede bilirubin excretion, leading to complications that require prompt evaluation and precise management.
Neonatal Hemolytic Disease
Blood group incompatibility sits at the center of neonatal hemolytic disease, a leading cause of severe hyperbilirubinemia that can escalate quickly without prompt recognition and treatment.
When a mother’s antibodies cross the placenta and attack the fetal red blood cells, hemolysis accelerates, bilirubin levels surge, and risks increase.
Rh incompatibility remains the classic trigger, and severe cases may progress to erythroblastosis fetalis, with anemia, hydrops, and distress.
You serve families best by recognizing early warning signs, insisting on timely testing, and ensuring appropriate intervention.
Antenatal screening, Coombs testing, and vigilant newborn monitoring are vital.
When indicated, phototherapy, intravenous immunoglobulin, or exchange transfusion can prevent kernicterus and lifelong injury.
If providers fail to adhere to standards or delay care, legal action may be necessary to ensure accountability and secure resources for long-term support.
G6PD Deficiency Triggers
Often overlooked until jaundice escalates, glucose-6-phosphate dehydrogenase (G6PD) deficiency can precipitate sudden, severe hyperbilirubinemia when oxidative stress triggers hemolysis. You should recognize that G6PD variants determine vulnerability, and even routine exposures can become dangerous.
Common oxidative triggers include sulfa antibiotics, nitrofurantoin, antimalarials, and high-dose aspirin. Naphthalene from mothballs, aniline dyes, and certain industrial chemicals can also provoke hemolysis.
Viral or bacterial infections, with associated fevers and inflammatory stress, frequently precipitate crises. Dietary exposures matter as well; fava beans are a classic cause of rapid red cell breakdown.
When hemolysis accelerates, bilirubin levels rise abruptly, necessitating prompt monitoring and intervention. You can protect families by identifying risks, documenting exposures, and ensuring that clinicians consider G6PD testing, especially in populations with a known prevalence. Early action prevents irreversible injury.
Breastfeeding-Associated Jaundice
While hemolytic triggers like G6PD deficiency can send bilirubin soaring, breastfeeding-associated jaundice remains a more common pathway to severe hyperbilirubinemia in otherwise healthy newborns.
You often see rising bilirubin when inadequate intake delays stooling, slowing bilirubin excretion. Latch-on challenges, painful feeds, or infrequent nursing can compound the risk, particularly in the first week. Milk supply myths may discourage early supplementation or timely lactation support, allowing levels to climb unnoticed.
As a caregiver or advocate, you should push for prompt assessment of feeding effectiveness, daily weight checks, and bilirubin monitoring using recognized nomograms. Hospitals must document intake and output, address dehydration, and arrange lactation consultation without delay.
When providers overlook red flags or dismiss parental concerns, preventable injury can follow, and legal accountability may be warranted.
Biliary Obstruction Complications
Even when a newborn appears well, biliary obstruction can rapidly drive bilirubin to dangerous levels and set the stage for irreversible harm. You must recognize that blocked ducts impede bile flow, allowing unconjugated and conjugated bilirubin to accumulate. Untreated, this condition risks kernicterus, coagulopathy, infection, and progressive liver injury.
Prompt imaging, fractionated bilirubin testing, and consultation with pediatric gastroenterology are crucial steps.
You should press for targeted interventions. Where appropriate, biliary stenting can restore drainage, relieve cholestasis, and prevent the escalation of toxicity. If gallstones or strictures cause obstruction, timely removal or dilation reduces the risk of recurrence. Monitor for complications such as cholangitis and cholestatic pancreatitis, which can destabilize infants quickly.
Document every delay, order, and result. By advocating decisively, you safeguard the child’s neurologic function and preserve future health.
Legal Rights of Severe Hyperbilirubinemia Injury Victims
Because severe hyperbilirubinemia can result from preventable medical errors, you may have legal rights to pursue compensation when providers fail to meet accepted standards of care.
You’re entitled to expect clinicians to follow hospital protocols, communicate urgent lab results promptly, and escalate care as needed. When lapses occur, the law allows you to pursue damages for medical costs, lost wages, and pain and suffering.
Effective patient advocacy supports your claim by documenting deviations from guidelines and showing how timely intervention would likely have prevented harm.
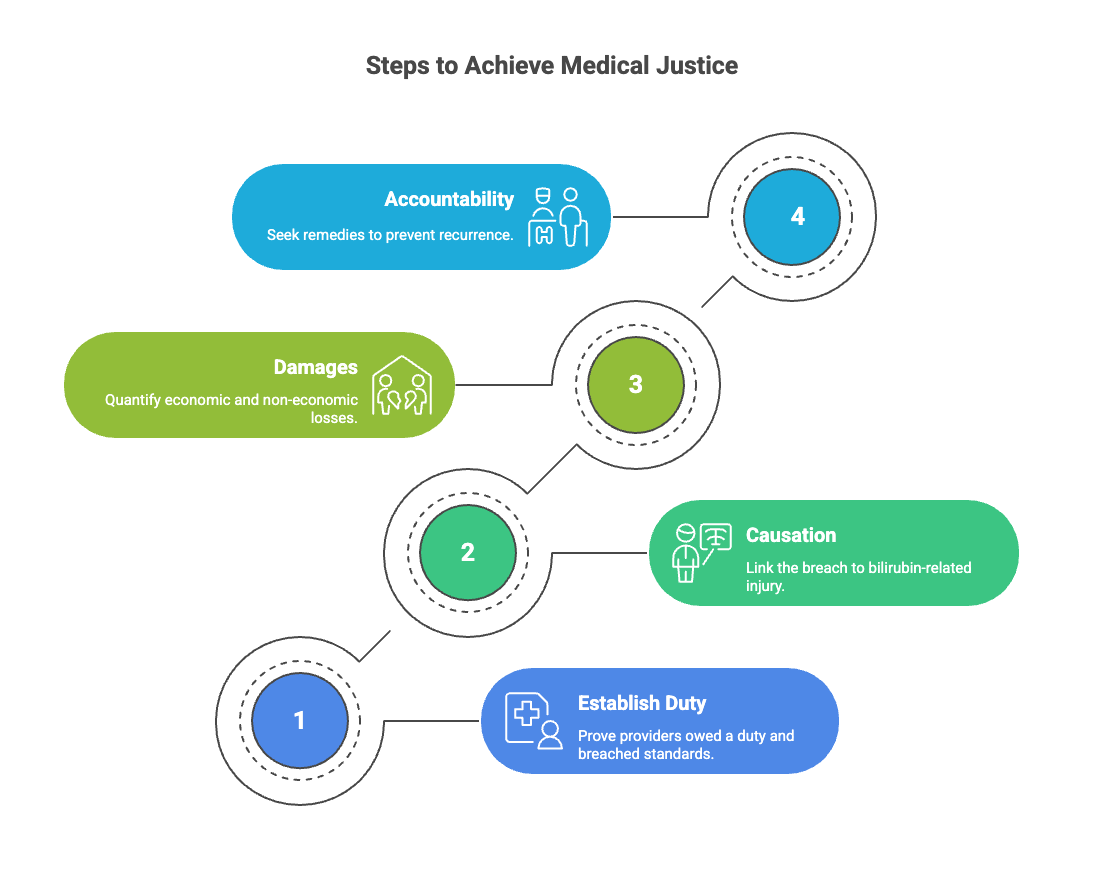
- Establish duty and breach: prove providers owed you a duty and violated standards through ignored symptoms, delayed tests, or protocol failures.
- Causation: link the breach to bilirubin-related injury, using expert testimony and medical records.
- Damages: quantify economic and non-economic losses, including future care and diminished quality of life.
- Accountability: seek remedies that promote safer hospital protocols, encourage staff training, and foster systems that prevent recurrence.
Steps to Take After a Severe Hyperbilirubinemia Injury
After a severe hyperbilirubinemia injury, you should seek immediate medical care to stabilize your condition and establish a clear clinical record.
Preserve all medical records, test results, discharge summaries, and communications, as these documents will be essential in evaluating causation and damages.
Consult an experienced attorney promptly, so you can protect your rights, meet deadlines, and position your claim for a thorough and strategic appraisal.
Seek Immediate Medical Care
At the first sign of severe jaundice, lethargy, poor feeding, high-pitched crying, or arching of the back, seek immediate medical care to protect your child from bilirubin-induced brain injury.
Go to the nearest emergency department or call your pediatrician’s urgent line, and clearly state your concern for acute hyperbilirubinemia. Request an emergency assessment, including prompt bilirubin testing, vital signs, and neurologic observation. Insist on timely treatment decisions based on hour-specific nomograms and risk factors.
Ask about phototherapy thresholds, hydration, and whether escalation to exchange transfusion is indicated.
Confirm that blood type incompatibility, hemolysis, infection, and dehydration are evaluated.
If transfer to a higher level of care is needed, authorize it without delay. Your swift, decisive action guarantees the team initiates proven interventions, minimizing the risk of kernicterus and long-term disability.
Preserve Medical Records
Swift medical action protects your child; now protect the record that proves what happened.
Gather complete medical documentation from every provider involved, including prenatal records, bilirubin levels, phototherapy logs, medication lists, nursing notes, and discharge summaries. Request copies promptly, note dates of request and receipt, and keep originals unmarked. Create a simple index so you can locate crucial entries quickly.
Secure redundant storage. Make clear, legible scans, label files by date and facility, and maintain digital backups on encrypted drives and reputable cloud services. Preserve metadata when possible, and store paper copies in a dry, secure location. Document all communications with hospitals and insurers, saving emails, portal messages, and voicemail transcriptions.
Consistent organization reduces disputes, supports timelines, and protects your child’s interests.
Consult an Experienced Attorney
Engage qualified legal counsel as soon as you recognize signs of severe hyperbilirubinemia injury or suspect lapses in care. An experienced attorney will evaluate the facts, identify liable parties, and preserve vital evidence. You’ll receive a focused client consultation that clarifies your legal options, timelines, and potential damages, allowing you to act decisively on behalf of the injured child.
Choose counsel with demonstrated neonatal injury experience and access to medical experts. Ask about case strategy, communication practices, and expected milestones. A contingency fee arrangement can reduce financial strain, ensuring you pay legal fees only if there’s a recovery.
Prompt legal guidance helps secure records, comply with notice requirements, and prevent costly mistakes. By retaining seasoned counsel, you protect the child’s future and advance accountability.
How a Severe Hyperbilirubinemia Injury Lawyer Can Help You
While medical providers should prevent and promptly treat dangerous bilirubin levels, a severe hyperbilirubinemia injury lawyer steps in to protect your rights when that duty fails. You get a strategic advocate who understands neonatal care standards, discharge protocols, and the consequences of missed screenings.
Your lawyer investigates records, consults experts, and identifies where systems and individuals deviated from required care.
With careful guidance, you can pursue accountability while maintaining focus on your child’s needs and recovery.
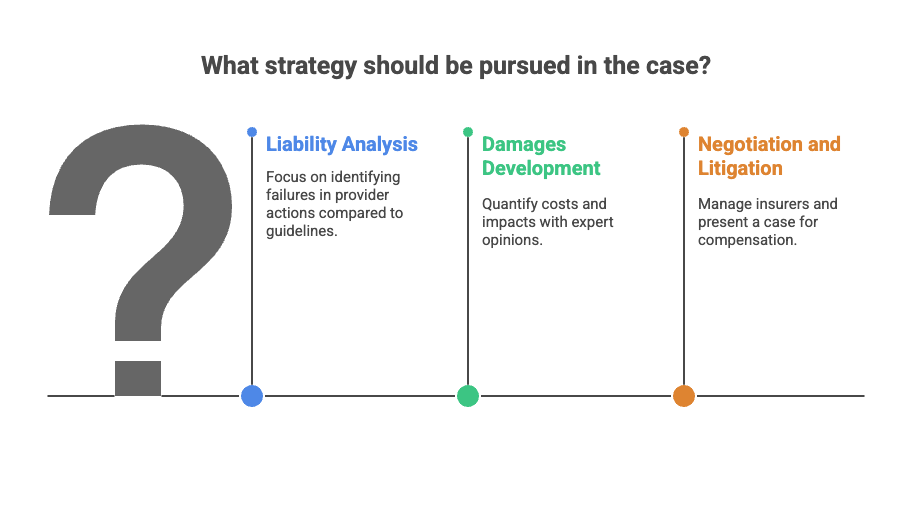
- Case evaluation and investigation: Your lawyer reviews charts, lab trends, and parental guidance documentation, then interviews witnesses and engages consultants.
- Liability analysis: They compare provider actions to established neonatal guidelines, flagging failures in monitoring, escalation, and informed consent.
- Damages development: They quantify medical costs, caregiving supports, and family impacts, supported by credible expert opinions.
- Negotiation and litigation: Your lawyer manages insurers, crafts evidence-driven demands, and, if needed, presents a clear case at trial to secure just compensation.
Long Term Effects of Severe Hyperbilirubinemia Injuries
You may face persistent neurological and cognitive impairments that affect memory, attention, and executive functioning, shaping daily living and long-term independence.
Motor and movement disorders, including muscle rigidity, tremors, and coordination issues, can limit mobility and require ongoing therapy.
Hearing and speech challenges may hinder language development and communication, necessitating early evaluation and targeted interventions.
Neurological and Cognitive Impairments
Although acute symptoms may fade, severe hyperbilirubinemia can leave lasting neurological and cognitive impairments that shape a child’s development and daily functioning.
You may observe challenges with attention, memory, language processing, and executive skills, which can hinder learning and social participation.
These issues often trace back to disrupted neonatal neurodevelopment, where bilirubin toxicity affects regions responsible for cognition and sensory integration.
Early identification is crucial.
Thorough neuropsychological evaluations, ongoing educational assessments, and careful care coordination help you target specific deficits.
Evidence-based interventions, including speech-language therapy, occupational strategies for cognitive support, and structured cognitive rehabilitation, can improve outcomes when delivered consistently.
You should also document needs and progress, ensuring schools and insurers provide appropriate services.
As legal advocates, we investigate lapses in monitoring and intervention, and seek resources to support lifelong care.
Motor and Movement Disorders
Because bilirubin neurotoxicity often targets the basal ganglia and cerebellar pathways, severe hyperbilirubinemia can lead to enduring motor and movement disorders that shape mobility and independence across the lifespan.
You may see abnormal tone, poor postural control, and involuntary movements that interfere with daily care and safe mobility. Infant dystonia, spasticity, and choreoathetoid movements often emerge early, and they may progress without timely interventions.
As a caregiver or advocate, you can monitor for regression in movement, delayed sitting or walking, and persistent head lag.
Structured therapy, orthopedic evaluation, and assistive technology can stabilize function and prevent avoidable complications.
When medical negligence contributed to the injury, you’re entitled to pursue resources for rehabilitation, equipment, and in‑home support, ensuring dignified mobility and minimizing secondary harm over time.
Hearing and Speech Challenges
While bilirubin primarily injures the auditory pathway deep within the brainstem, its effects extend outward, creating lasting hearing and speech challenges that demand vigilant management.
You may experience auditory neuropathy, where sound reaches the inner ear but neural signaling becomes disordered, resulting in fluctuating hearing and poor speech discrimination. Infants can pass newborn screenings yet struggle later with processing speech, particularly in noisy environments. Early diagnostic testing, including ABR and otoacoustic emissions, helps confirm the pattern and guide intervention.
You can support language development through coordinated services: timely amplification or cochlear implants, auditory-verbal therapy, and consistent speech-language therapy. Prioritize routine audiology monitoring, individualized education plans, and caregiver training.
Document services, progress, and missed opportunities, as records substantiate causation and damages. Acting early preserves communication, learning, and social participation.
Proving Liability in Severe Hyperbilirubinemia Medical Malpractice Injury Cases
Proving liability in a severe hyperbilirubinemia malpractice case hinges on establishing a transparent chain of duty, breach, causation, and damages, supported by authoritative medical standards.
You begin by identifying who owed your child a duty of care, including physicians, nurses, and facilities responsible for screening, monitoring, and timely intervention. Next, you show breach by comparing their actions to neonatal guidelines on bilirubin assessment and treatment.
You then connect that breach to the injury through precise medical documentation and expert testimony. Chart notes, bilirubin levels, risk assessments, discharge instructions, and follow-up orders help demonstrate what should’ve been done and when. Independent neonatology and nursing experts translate these records into explicit opinions on preventability and missed opportunities.
Finally, you prove damages by linking the bilirubin-related injury to functional losses and necessary supports. We want you to know that throughout this process, you act with diligence and integrity, ensuring every assertion rests on verifiable data and recognized standards, so accountability aligns with compassionate advocacy.
Compensation for Severe Hyperbilirubinemia Damages
Although no amount of money can undo a bilirubin-related brain injury, compensation in severe hyperbilirubinemia cases aims to secure your child’s long-term care and restore financial stability. A well-constructed recovery should address medical expenses already incurred, ongoing therapies, adaptive equipment, and specialized nursing or attendant services.
You can also seek funds for home modifications, transportation needs, and educational supports that promote development and independence.
Damages typically include projected costs for lifelong treatment, lost earning capacity, and the value of in-home caregiving you provide. Pain and suffering, loss of enjoyment of life, and the family’s need for emotional support are compensable as well, recognizing the profound, daily impact of kernicterus-related disabilities. In appropriate cases, you may recover the cost of case management and coordinated care planning, ensuring continuity and safety.
Your attorney should present detailed life-care planning, credible medical opinions, and economic analyses, translating clinical needs into concrete dollar figures that fully fund long-term care.
The Statute of Limitations for Severe Hyperbilirubinemia Injury Cases
Because deadlines can quietly determine the fate of your claim, you must understand the statute of limitations that governs severe hyperbilirubinemia injury cases. Each state sets a filing period, often two to three years, and missing it can end your case before it begins.
You should identify the applicable statute early, confirm whether it’s a medical malpractice or general negligence timeline, and calendar every critical date.
Many jurisdictions recognize the discovery rule, which starts the clock when you knew or reasonably should’ve known the injury and its cause. In neonatal cases, late discovery may occur when developmental delays or kernicterus are diagnosed months or years later. You must also assess tolling exceptions. These can pause the deadline for minors, incapacitated persons, fraudulent concealment, or ongoing treatment in some states.
Track pre-suit notice requirements, expert affidavit mandates, and government claim procedures, which can shorten timelines. Document symptoms, evaluations, and provider communications to preserve evidence and timing.
Why You Need an Experienced Severe Hyperbilirubinemia Injury Lawyer
When a newborn suffers severe hyperbilirubinemia, you face complex medical questions, high-stakes damages, and unforgiving procedural rules that demand seasoned legal guidance. You need experienced counsel that understands neonatal standards of care, bilirubin monitoring protocols, and how missed interventions lead to kernicterus and lifelong disability.
An attorney with focused experience can secure and interpret medical records, consult qualified experts, and build a causation narrative that withstands scrutiny.
You also need a strategist who quantifies future care, specialized therapies, assistive technology, and educational services, converting needs into defensible damages. Strong parental advocacy is crucial; a skilled lawyer elevates your voice, coordinates with care teams, and protects your child’s rights in every forum.
Insurers and hospitals deploy sophisticated defenses, so your lawyer must anticipate tactics, preserve evidence, and meet every deadline. With disciplined case management, precise negotiations, and trial-ready preparation, you safeguard accountability and obtain resources your child requires now and for life.

How to Choose the Right Severe Hyperbilirubinemia Injury Lawyer for Your Case
Securing the right attorney follows naturally after recognizing what’s at stake in a severe hyperbilirubinemia case. You need counsel who understands neonatal medicine, hospital protocols, and causation standards, and who can translate that knowledge into decisive action. Start with targeted research, then verify licensure, disciplinary history, verdicts, and settlements in similar cases.
Conduct a structured Client interview. Ask how the lawyer evaluates bilirubin charts, phototherapy timing, exchange transfusion criteria, and follow-up documentation. Request examples of expert networks, including neonatologists and pediatric neurologists, and clarify who’ll handle day-to-day strategy and communication.
Examine the Fee structure with care. Confirm contingency percentages, litigation costs, expert fees, and whether expenses are deducted before or after the contingency is calculated. Demand written disclosures and a clear budget for discovery and trial.
Assess bandwidth and timelines. Determine caseload, projected milestones, and trial readiness. Finally, choose the advocate who offers transparent counsel, disciplined preparation, and a service mindset aligned with your commitment to the child’s wellbeing.
About the Law Offices of Anidjar and Levine
Founded on disciplined advocacy and meticulous case preparation, the Law Offices of Anidjar and Levine provides all-encompassing representation for families confronting severe hyperbilirubinemia injuries. You’ll work with a team that aligns legal strategy with your goals, prioritizing accountability, safety, and long-term support for your child.
The firm structures each case around clear evidence, expert testimony, and proactive negotiation, while preparing for trial from day one.
You can review client testimonials to understand how the firm maintains responsive communication and reliable guidance during intricate medical-legal disputes. Their firm history reflects steady growth built on results, professional integrity, and service to vulnerable families. You’ll receive attentive counsel, consistent updates, and transparent expectations about timelines and outcomes.
The attorneys coordinate with medical consultants, evaluate lifetime care costs, and protect your rights against insurers and institutional defendants. With disciplined case management and focused advocacy, the firm seeks meaningful resolutions that provide funding for care, restore dignity, and promote community safety.
You deserve decisive guidance after a severe hyperbilirubinemia injury. With experienced counsel, you’ll understand your rights, preserve critical evidence, and meet strict deadlines while building a compelling claim.
We coordinate experts, analyze neonatal care, and quantify lifetime needs to pursue full compensation through negotiation or litigation.
Don’t wait—early action strengthens your case and protects your child’s future.
Contact the Birth Injury Lawyer team at the Law Offices of Anidjar and Levine for a thorough evaluation and strategic advocacy tailored to your family’s circumstances.

